
Quality and safety are increasingly important in medicine because systems are focused on delivering better value and outcomes to patients and payors. However, even with the many checks and balances being introduced into clinical workflows, clinical teams are still facing a challenge to deliver consistent, evidenced-based best practices at the point of care.
While radiological procedures may usually seem nonlife-threatening, there is still considerable risk -- real or perceived. Certainly, invasive interventional procedures do carry significant risk, even death (i.e., angiography or percutaneous biopsy). Other procedures have theoretical risks, such as the effects of radiation dose exposure (even at lower doses) mainly from CT. Furthermore, there is widespread variation in the use of appropriate examinations (imaging tests) for a particular condition, sometimes referred to as appropriateness.
Despite much evidence about the use of appropriate best practices for radiological procedures, variation in the practice of radiology abounds, usually with no two departments alike delivering similar practices and operating procedures. What might seem appropriate in one department is often not seen as inappropriate in another -- for instance, what is viewed as an acceptable radiation dose varies across regions, towns, and sometimes even within the same health organization.
Demands from patients
Patients themselves are now demanding better outcomes and less variation, particularly as it has become more evident from the press that outcomes can significantly vary from one organization to another. This has come at a time when demand for imaging services is busier than ever as referrers continue to see imaging as a key tool to reach a diagnosis earlier, monitor therapy more closely, and/or cure and palliate patients through innovative interventional therapies.
Quality and safety measures, which are often difficult to measure, let alone deemed as meaningful in the first place, are then sometimes seen as an afterthought. Considering the numerous other nonremunerated regulatory and compliance measures required from radiologists, quality and safety initiatives are often viewed as overly burdensome and are relegated to the domain of just "doing the right thing" for the patient rather than a compelling reason to do so.
Despite these challenges and the increasing nonclinical workload that radiologists are facing, it is imperative that all caregivers and departments develop, implement, and monitor a robust quality and safety program to remove unnecessary variation, deliver best practices at the point of care, and ultimately deliver better outcomes for their patients. Achieving this requires a cultural shift within the organization, sometimes referred to as the "culture of safety." This starts with leadership whose role it is to impart a compelling reason to their staff as to why quality and safety is integral to every aspect of the workflow, why measurement is important, and why change is mandatory when standards do not meet best practices.
As with all leadership, effective translation of the vision will require choosing the right teams to develop meaningful strategies, tactics, and tools to deliver better quality. These teams need to work with the wider department to ensure consistent delivery of the solutions.
Once leadership provides the vision for the quality and safety agenda, it is advantageous to frame the approach by considering the operations in totality rather than piecemeal, where individual activities are not viewed as connected or integrated into a larger framework.
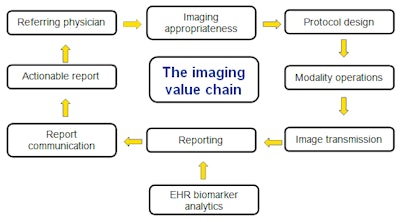 The value chain can be viewed as the workflow from when a referrer orders an exam to when a report is received. EHR = electronic health record.
The value chain can be viewed as the workflow from when a referrer orders an exam to when a report is received. EHR = electronic health record.The imaging value chain (see figure) can be simplistically imagined as the workflow from when a referrer orders an imaging test to when he or she receives a report, hopefully one that is actionable. Ideally, the referring doctors are familiar with the right test to order for the patient (image appropriateness), but often they do not know precisely the best test to order at that time for a patient. This can be termed imaging inappropriateness, with some believing this could account for up to 30% of all imaging requests.
 Dr. Giles Boland.
Dr. Giles Boland.Once the test is ordered, it then needs to be scheduled and protocoled. Then the patient arrives at the imaging suite, and the procedure is performed. This could be either diagnostic or interventional. The images are acquired, transmitted, and stored, at which point the radiologist interprets the images -- with increasing access to collateral biomarker data residing in electronic health record databases. The reports are then communicated to the referring physician, and they should be succinct, structured, precise, unambiguous, and directional -- in other words, a report that the referrer can then use to determine the next best course of action without unnecessary additional tests or actions that might only lead to additional waste and cost in the system.
Quality and safety should not just be framed, as it frequently is, around events that lead to obvious immediate harm (i.e., contrast reactions or interventional complications). Rather they should be framed around the myriad of unique activities that constitute the overall radiology workflow. Many of these activities may, in themselves, seem trivial as to their contribution to risk and adversity (such as the recommendation for an unwarranted test or minor variations in MRI protocol design), but in aggregate these variations can lead to considerable costs and even harm.
 Dr. Lluís Donoso-Bach.
Dr. Lluís Donoso-Bach.Until radiologists recognize that it is the responsibility of the overall team to evaluate every operational activity to determine if it meets best practice standards, quality and safety efforts will be undermined and sometimes ineffective. It is the role of leadership to frame the issues of importance to their departments and then to build the teams to create, deliver, and manage solutions using data-driven management techniques and the necessary tools and resources to perpetually drive toward better practices and outcomes.
Dr. Giles Boland is a professor of radiology at Brigham and Women's Hospital in Boston, Massachusetts, U.S. Dr. Lluís Donoso-Bach is a professor of radiology at Hospital Clínic of Barcelona in Barcelona, Spain. Their book, Quality and Safety in Imaging, was published this year by Springer.



















