Most experts recommend MRI for patients with a history of systematic negative biopsies and in whom there is still a suspicion of prostate cancer, but the added value remains controversial, Dr. Olivier Rouvière, PhD, told delegates at the French national radiology congress (Journées Francophones de Radiologie Diagnostique et Interventionnelle, JFR 2018).
Thanks to its excellent sensitivity, multiparametric MRI is increasingly used to define suspicious zones before a prostate biopsy. This allows doctors to add "targeted biopsies" to systematic classic biopsies that cross the gland blind.
Thus MRI is recommended by most scientific societies for patients with a history of systematic negative biopsies and in whom there is still a suspicion of prostate cancer. This population mostly has tumors in the zones undersampled by systematic biopsy (anterior half, extreme base, or extreme apex). On the other hand, the added value of targeted biopsies remains debated in patients undergoing a first series of biopsy.
Two recent studies have just changed the landscape, however.
The PRECISION study -- a prospective international multicenter study -- randomized 500 patients undergoing a first round of prostate biopsy. Half had systematic biopsy (10 to 12 samples) without MRI, while the other half had MRI and no biopsy if the MRI was negative (PI-RADSv2 ≤ 2) and only targeted biopsies (up to three targets and four samples per target) if the MRI was positive.
The detection rate of Gleason cancer score ≥ 7 was significantly higher in the MRI group (38% versus 26%, p = 0.005). The detection of clinically nonsignificant cancers (Gleason 6) was significantly lower in the MRI group (9% versus 22%, p ≤ 0.001). Some experts have immediately concluded that one can just conduct a targeted biopsy, with the double advantage of it detecting more aggressive cancers and fewer nonsignificant cancers.
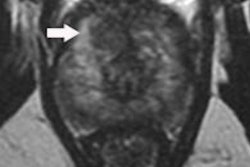
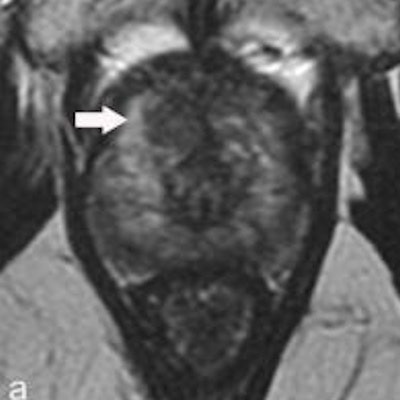
![Multiparametric MRI performed in a 59-year-old patient presenting with dysuria and a family history of prostate cancer (a = T2-weighted image, b = diffusion-weighted image at 2,000 sec/mm2, c = apparent diffusion coefficient [ADC] map, d = dynamic image obtained after injection of gadolinium chelates). The rate of prostate-specific antigen was 2.2 ng/mL. Digital rectal examination found a nodule to the left. MRI showed a suspicious lesion with a score of PI-RADS 4 (arrow) in the anterior horn of the right apex. Systematic biopsies (12 samples) were negative. Biopsies targeting the MRI lesion showed prostate cancer with a Gleason score of 8 (4 + 4). Figure courtesy of Dr. Olivier Rouvière, PhD, republished from E-Quotidien des JFR.](https://img.auntminnieeurope.com/files/base/smg/all/image/2018/10/ame.2018_10_15_20_04_2196_2018_10_16_JFR_irm_multiparametrique.png?auto=format%2Ccompress&fit=max&q=70&w=400) Multiparametric MRI performed in a 59-year-old patient presenting with dysuria and a family history of prostate cancer (a = T2-weighted image, b = diffusion-weighted image at 2,000 sec/mm2, c = apparent diffusion coefficient [ADC] map, d = dynamic image obtained after injection of gadolinium chelates). The rate of prostate-specific antigen was 2.2 ng/mL. Digital rectal examination found a nodule to the left. MRI showed a suspicious lesion with a score of PI-RADS 4 (arrow) in the anterior horn of the right apex. Systematic biopsies (12 samples) were negative. Biopsies targeting the MRI lesion showed prostate cancer with a Gleason score of 8 (4 + 4). Figure courtesy of Dr. Olivier Rouvière, PhD, republished from E-Quotidien des JFR.
Multiparametric MRI performed in a 59-year-old patient presenting with dysuria and a family history of prostate cancer (a = T2-weighted image, b = diffusion-weighted image at 2,000 sec/mm2, c = apparent diffusion coefficient [ADC] map, d = dynamic image obtained after injection of gadolinium chelates). The rate of prostate-specific antigen was 2.2 ng/mL. Digital rectal examination found a nodule to the left. MRI showed a suspicious lesion with a score of PI-RADS 4 (arrow) in the anterior horn of the right apex. Systematic biopsies (12 samples) were negative. Biopsies targeting the MRI lesion showed prostate cancer with a Gleason score of 8 (4 + 4). Figure courtesy of Dr. Olivier Rouvière, PhD, republished from E-Quotidien des JFR.The MRI-FIRST study -- a prospective multicentric French study -- slightly curbs this enthusiasm. It included 275 patients undergoing a first round of prostate biopsy. All had an MRI scan then systematic biopsies (12 to 14 samples) carried out by a practitioner who had not seen the MRI results, then targeted biopsies (up to two targets and three samples per target) by another practitioner; if the MRI was negative (Likert ≤ 2), the patient only underwent systematic biopsy.
In the MRI-FIRST study, the targeted biopsies detected more cancers with a Gleason score of ≥ 7, but the difference was a lot smaller than in the PRECISION study and nonsignificant (32.3% versus 29.9%, p = 0.38). The detection rate obtained by the combination of systematic and targeted biopsies was 37.5%. Cancers with Gleason score ≥ 7 were missed in 7.6% of patients without targeted biopsies and in 5.2% of patients without systematic biopsy. The targeted biopsies detected significantly fewer nonsignificant cancers (Gleason 6 and maximum length diseased < 6 mm; 5.6% versus 19.5%, p < 0.0001).
 Dr. Philippe Puech speaks at JFR 2018.
Dr. Philippe Puech speaks at JFR 2018.MRI-FIRST also looked at the detection rate for cancers with Gleason score ≥ 7 (4 + 3), and it was significantly higher for targeted biopsies (19.9% versus 15.1%, p = 0.0095).
Get to know PI-RADS
All radiologists should know the PI-RADS scoring system by heart when interpreting prostate MRI, Dr. Philippe Puech, professor of radiology at Lille University Hospital, told JFR 2018 delegates in Paris. Furthermore, perfect knowledge of the complex prostate anatomy is also necessary for analyzing and scoring the images, he said.
During the session, the use of postcontrast dynamic imaging series was promoted for improved detection and characterization of prostate cancer, although this approach is not uniformly followed yet.
Dr. Raphaele Renard Penna, a radiologist from the Pitié Salpêtrière Hospital in Paris, spoke about the importance of staging of prostate cancer. The role of radiologists extends beyond the detection and identification of cancer in the prostate by MRI, she said. They should also stage systematically because it significantly influences the strategy of treatment and surgical technique performed by urologists. For example, if the capsule of the prostate is perforated, then another type of surgery can be performed with less risk of erectile dysfunction afterwards for the patient.
The new guideline from the French Society of Urologists regarding indications for prostate MRI is due to be published in November and states that prostate MRI should be the first examination in all cases, before biopsy is performed, she pointed out.
Renard Penna also told JFR attendees about the errors that can occur when interpreting prostate MRI scans.
So what can we conclude from this research?
The two studies prove that an MRI performed before biopsy increases the detection rate of cancers with Gleason score ≥ 7, even in patients without previous history of biopsy. It is therefore probable that soon it will be recommended before all prostate biopsies.
Even if it is desirable to eliminate systematic biopsies to reduce the overdiagnosis of nonsignificant cancers, the results of the MRI-FIRST study call for prudence. The number of targeted samples and the quality of their guidance are also in the spotlight. In MRI-FIRST, there were fewer targeted samples than in PRECISION. Yet, in the 13 patients from the MRI-FIRST study in whom systematic biopsy detected a cancer with a Gleason score ≥ 7 missed by the MRI/targeted biopsy duo, five had a negative MRI; the eight others had an MRI target in the lobe (five in the sextant) where the systematic biopsies were positive.
It is possible that for certain patients, targeted biopsies missed a cancer correctly localized by MRI. The number and the ideal guiding of targeted samples therefore remains to be defined in line with the size of the target and the volume of the prostate.
Finally, the necessity to perform MRI before each prostate biopsy poses a double challenge for the radiological community: a quantitative challenge, given the saturation of machine availability in France, but also a qualitative challenge, in light of the great interreader variability of MRI. Therefore, a large training effort will be necessary in the years to come.
Dr. Olivier Rouvière, PhD, is professor of radiology at the department of genitourinary and vascular radiology at Hôpital E. Herriot in Lyon, France.
Editor's note: This is an edited translation of an article published in French on 13 October 2018 by E-Quotidien des JFR, the daily electronic news outlet of the JFR. Translation by Frances Rylands-Monk.