Prostate artery embolization (PAE) has emerged as a promising treatment for lower urinary tract symptoms secondary to benign prostatic hypertrophy (BPH). This article provides an up-to-date overview of this minimally invasive technique, including discussion of potential benefits, patient selection, and technical challenges.
Current evidence suggests PAE is an effective option for patients with large prostate volume and multiple comorbidities, as well as for younger patients with medication-induced erectile dysfunction and suboptimal results from pharmacotherapy. However, larger randomized studies with long-term follow-up data are needed for this technique to be formally established in the treatment regime for benign prostatic hypertrophy.
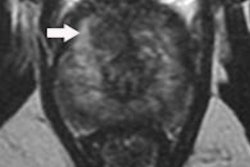
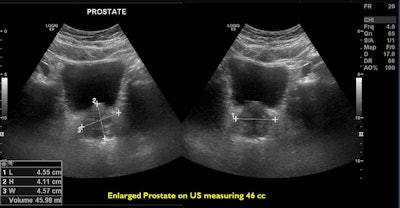 A 66-year-old patient with an International Prostate Symptom Score (IPSS) of 29 and prostate volume of 46 cc. All images courtesy of Dr. Jamal Al Deen Alkoteesh.
A 66-year-old patient with an International Prostate Symptom Score (IPSS) of 29 and prostate volume of 46 cc. All images courtesy of Dr. Jamal Al Deen Alkoteesh.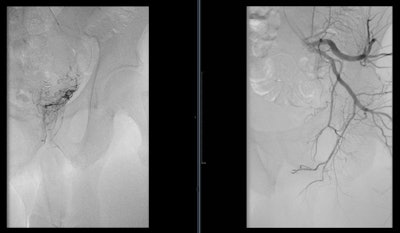 Angiogram of the left internal iliac artery showing the origin of the left prostatic artery and then very selective catheterization of the left prostatic artery by microcatheter.
Angiogram of the left internal iliac artery showing the origin of the left prostatic artery and then very selective catheterization of the left prostatic artery by microcatheter.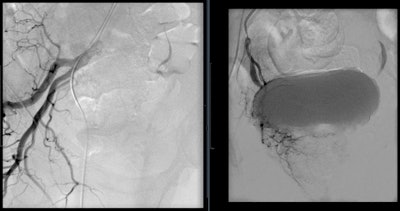 Angiogram of the right internal iliac artery showing the origin of the right prostatic artery and then very selective catheterization of the right prostatic artery by microcatheter.
Angiogram of the right internal iliac artery showing the origin of the right prostatic artery and then very selective catheterization of the right prostatic artery by microcatheter.How the treatment works
As men age, the prostate gland grows larger and may begin to press on the urethra. Enlarged prostate affects more than half of men by age 60 and causes symptoms such as frequent urination, weak urine stream, and a persistent feeling of having to urinate. Surgery is the standard treatment for the condition, but it can cause complications such as sexual dysfunction.
Prostate artery embolization is a noninvasive procedure that can bring long-term relief from symptoms caused by an enlarged prostate. This procedure works by closing the blood supply to the prostate, and, as a result, the prostate shrinks in size, reducing blockages and improving the symptoms.
PAE is an option for patients with a variety of prostatic issues, including lower urinary tract symptoms secondary to benign prostatic hypertrophy, hematuria of prostatic origin, and prostate cancer. After initial medical therapy, transurethral resection of the prostate (TURP) remains the gold standard surgical treatment, but its role is undermined by the associated risks of bleeding and lasting sexual dysfunction.
With the considerable prevalence of BPH and an associated impact on national healthcare in the United Arab Emirates (UAE), less-invasive options and minimally invasive procedures have been continually examined. Since performing the first PAEs in 2008, the multidisciplinary team at the University of São Paulo in Brazil has been encouraged by patient outcomes. Al Ain Hospital has been offering PAE since 2015, and more than 25 patients with BPH have been treated.
 Dr. Jamal Al Deen Alkoteesh conducts an interventional procedure at Al Ain Hospital in the United Arab Emirates.
Dr. Jamal Al Deen Alkoteesh conducts an interventional procedure at Al Ain Hospital in the United Arab Emirates.Coping with technical challenges
Technically, PAE is challenging. Unnecessary catheterization increases procedure time and radiation exposure. Knowledge of anatomical features to identify and catheterize target arterial branches is paramount to achieve the best clinical outcomes. The prostate receives its arterial supply via the medial and the capsular/lateral branches but is variable among patients.
Assis et al proposed an angiographic classification of prostate artery anatomy and analyzed 286 pelvic sites to find that most inferior vesical arteries and their prostatic branches arise from the internal pudendal artery. Conebeam CT (CBCT) angiography has been utilized to evaluate the many variants of the prostatic artery. With direct contrast injection and 3D angiography, subtle prostatic feeders are better identified when compared with digital subtraction angiography and CT angiography.
Traditionally, PAE has been performed via a transfemoral approach (TFA), but the transradial approach (TRA) has garnered increased interest recently. Evidence has suggested that TRA results in shorter postprocedure hospital stays, decreased access-site complications, and improved patient satisfaction. This method would also allow patients to ambulate immediately post-PAE, which could facilitate urination. The distance from the forearm to pelvis along with the arterial tortuosity and previously mentioned variant anatomy has deterred initial attempts for PAE via TRA. Further, prior to selecting TRA patients, collateral circulation must be adequate as determined using a Barbeau test (i.e., a modified Allen test with a pulse-oximetry device).
Studies show that when PAE is performed via TRA, patients don't need pre-PAE pelvic angiograms and have decreased procedure times, fluoroscopy times, and total radiation doses when compared with PAE through TFA. The exclusion criteria for TRA-PAE has been patient height, type D Barbeau waveform, and radial artery diameter less than 2.0 mm.
One of the most promising benefits of PAE has been its efficacy in a variety of patient populations. PAE has been performed in patients with both small and large prostates. TURP in larger gland sizes, especially with prostate volumes larger than 80 cm, is associated with longer operative times and an increased risk of bleeding and anesthesia-related complications. In contrast, PAE has been demonstrated to be safe and efficacious in varying prostate sizes with no major complications.
Further, PAE has demonstrated its role in elderly patients (≥ 75 years old). In a prospective study done by Wang et al -- despite this cohort of patients having a higher prevalence of hypertension, heart disease, chronic obstructive pulmonary disease, urinary retention, and antiplatelet agent use than younger patients -- they experienced no major complications and a significant improvement in International Prostate Symptom Score (IPSS) after PAE. Conversely, TURP has been associated with an increased risk of complications in patients with multiple comorbidities.
In terms of symptomatic improvement in patients with lower urinary tract symptoms, PAE has continued to demonstrate its value. Most recently, a meta-analysis by Cizman et al examined PAE in the setting of short- to midterm follow-up. More than 500 PAE patients were assessed to determine the efficacy and safety of the procedure. At 12 months, IPSS and quality of life score decreased by 59% and 56%, respectively, with no significant change in International Index of Erectile Function scores. Prostate-specific antigen (PSA) level and postvoid residual (PVR) volume had the largest decrease within the first six months after PAE. Urinary peak flow rate also increased by more than 90% at 12 months. The analysis suggests that the degree and rate of morbidity associated with PAE are more favorable than that of TURP. When compared with adverse events of TURP, PAE has a lower incidence of bleeding, blood transfusion, urinary tract infections, and urethral stricture. PAE has also been demonstrated to have a minimal association with ejaculatory and erectile dysfunction when compared with TURP.
Pisco et al recently analyzed medium- and long-term outcomes post-PAE; 630 patients were examined at 18 to 78 months. Medium-term follow-up was defined as 18 to 36 months, and long-term follow-up was defined as 36 to 78 months. Long-term follow-up patients had a 76.3% success rate with a lack of sexual dysfunction or urinary incontinence. Most clinical failures occurred prior to 18 months post-PAE, the study authors noted. As time post-PAE increased, the incidence of clinical recurrence decreased. Among all patients, there was a mean improvement in IPSS, quality of life, and erectile function at both medium- and long-term follow-up. Correspondingly, prostate volume and PSA decreased during these time frames.
At Al Ain Hospital, we have seen patients improving within days of the procedure, some of them weeks, and one patient took one month until removal of the catheter.
PAE and hematuria
Prostatic hematuria is usually associated with BPH, iatrogenic urological trauma, or radiation therapy. Traditionally, it is treated conservatively with increased fluid intake, indwelling catheterization with bladder irrigation, and medical therapy. However, when these interventions fail, refractory hematuria is life-threatening. PAE has been shown to be an option for these patients. Although distinct prostatic hemorrhage is rarely seen on angiography, PAE is successful by obtaining complete arterial occlusion. By utilizing a superselective approach, control or cessation of hematuria within one to three days is achieved in 83% to 100% of patients.
After skin cancer, prostate cancer is the most common cancer affecting men in the U.S. Patients with advanced prostate cancer can present with or develop gross hematuria, urinary obstruction, and ureteral obstruction. Conventionally, this is treated with hormonal and other pharmacologic therapy. In refractory cases, surgical interventions have been performed. Although a large-scale trial has not yet been performed, PAE may play a role in the treatment of prostatic hemorrhage related to advanced prostate cancer.
Increased prostate volume has been associated with an increase in urinary complications postprostatectomy. In this sense, PAE may serve as a bridge to decrease prostate size and improve symptoms prior to prostatectomy or other surgical options.
Possible complications
Although the complications are minimal, PAE has adverse effects postprocedure. For patients without indwelling catheters, urethral burning during voiding and frequent urination have been the most common symptoms after PAE. However, these effects usually resolve within a week and can be treated with nonopioid analgesic medications. More serious complications are associated with nontarget embolization to the bladder, rectum, and penis. Ischemia to these organs is always possible and must be avoided through proper mapping via CBCT, microcatheterization for distal embolization, and calibrated microspheres for predictable embolization.
At Al Ain Hospital, three patients experienced complications, but the problems resolved within a few days. One patient had a 3-mm penile ulcer, which was treated by local antibacterial cream (Fucidin), while a second patient had hematospermia that resolved in two weeks. The last patient, a 54-year-old man, experienced "trash foot" from cholesterol emboli two days after the procedure. Doppler ultrasound showed a patent arterial tree with all runoff, and the foot improved by conservative management with aspirin 100 mg daily.
Looking to the future
PAE is a novel and promising therapy, and it has proved to be effective in treating BPH in symptomatic patients regardless of the size of the prostate. We have seen an increase in the number of self-referred patients coming to our interventional radiology clinic enquiring about this procedure, as they might have heard or read about it and wanted to avoid surgical options if possible. The latest results of PAE are similar to surgery but with fewer complications, and patients are getting discharged within three to six hours after the treatment with almost immediate symptom relief.
PAE could eventually become standard treatment for an enlarged prostate. It must be continually investigated to validate these encouraging observations. Future larger studies with long-term follow-up along with randomized control trials are currently underway. Although current data suggest that PAE is a promising procedure for interventional radiologists, a concerted effort to include a multidisciplinary team of urologists, diagnostic radiologists, and interventional radiologists will provide patients with optimum care.
Dr. Jamal Al Deen Alkoteesh is the chair of the radiology department at the Clinical Imaging Institute and chief medical officer, physician-radiology, at Al Ain Hospital in the United Arab Emirates.
Editor's note: This is an edited version of an article that originally appeared in the 31 January edition of the Arab Health 2019 daily newspaper. Dr. Alkoteesh was due to speak about "Vascular erectile dysfunction imaging and intervention" on 31 January as part of the Total Radiology conference at Arab Health 2019. References available on request.