Flat-panel CT (FPCT) of the temporal bone yields higher image quality than 128-slice CT with comparable overall effective doses, according to an Italian study published in the September edition of the European Journal of Radiology. Furthermore, the technique can be achieved on a flat-panel angiography system, rather than a dedicated flat-panel CT scanner.
 Dr. Giorgio Conte.
Dr. Giorgio Conte.The research has bolstered confidence in flat-panel CT as the gold standard for temporal bone assessment, according to a member of the research group from the University of Milan and the Fondazione IRCCS Ca'Granda Ospedale Maggiore Policlinico. The researchers first became aware they could use the hospital's flat-panel angiography system for cross-sectional imaging assessment of the temporal bone three years ago, via a study about image quality and radiation dose that compared flat-panel CT and conventional 64-slice CT.
"The results were brilliant, both in terms of image quality and dose, so FPCT was definitively introduced in our clinical practice. However, when a new dual-source 128-slice CT machine was installed in our department, we wondered if the gain in FPCT's image quality and dose was still present," said co-author and neuroradiologist Dr. Giorgio Conte from the polyclinic's neuroradiology unit.
"In the current study, we demonstrated the overall image quality of FPCT is higher than 128-slice CT without difference in dose. The effective dose was 0.5 mSv to0.6 mSv for both examinations acquiring both ears, but this result is even more significant considering the flat-panel angiography system, unlike multidetector CT [MDCT], allows us to scan only one ear, further reducing the dose by half -- about 0.2 mSv to 0.3 mSv," he said.
The key findings of the study are shown in the table below:
| Image quality score & effective dose for flat-panel CT & MDCT | ||
| flat-panel CT | 128-slices MDCT | |
| Overall score for image quality (min-max: 0-192 points)* |
173 (172.5-177.5) | 141 (137.5-144.0) |
| Effective dose (mSv)** | 0.58 | 0.56 |
** Dose was estimated by an anthropomorphic Rando Alderson phantom (Rando Alderson Research Laboratories, New York City, New York). Source: Dr. Giorgio Conte.
Specimen studies
The group imaged 16 anonymous and donated temporal bone specimens of normal hearing patients with both flat-panel CT and MDCT. The group then analyzed the images of 15 specimens for quality, after one specimen was excluded due to prior surgical removal of middle ear structures (EJR, September 2018, Vol. 106, pp. 106-113).
MDCT examinations were performed with a 128-slice CT scanner (Somatom Definition Flash, Siemens Healthineers) with a scan length 21 seconds. Images were reconstructed by using a standard filtered back projection algorithm with a high-resolution kernel (U70) and a slice thickness of 0.5 mm.
Flat-panel CT was performed with a C-arm angiographic system (Allura Xper FD20, Philips Healthcare), including a 30 x 40-cm digital flat-panel detector. The flat-panel CT scanning parameters were preset on the angiographic unit for the acquisition mode designed for the assessment of intracranial stents. Images were reconstructed with a slice thickness of 0.14 mm. The average reconstruction time for flat-panel CT images was approximately 10 minutes.
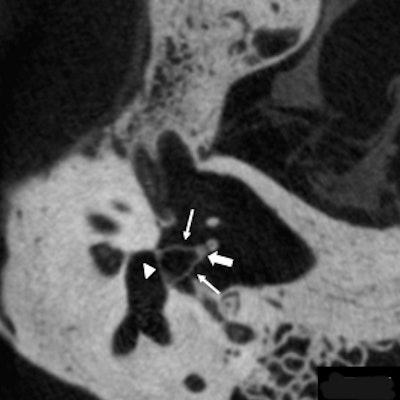
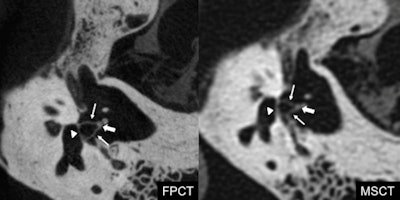 Footplate of the stapes (arrowhead), anterior and posterior crus (arrows), and head of the stapes (thick arrow). Flat-panel CT depicts all the components of the stapes better compared with multidetector CT, thanks to its higher spatial resolution and smaller field-of-view, which allows a magnified view. Courtesy of Dr. Giorgio Conte.
Footplate of the stapes (arrowhead), anterior and posterior crus (arrows), and head of the stapes (thick arrow). Flat-panel CT depicts all the components of the stapes better compared with multidetector CT, thanks to its higher spatial resolution and smaller field-of-view, which allows a magnified view. Courtesy of Dr. Giorgio Conte.Two neuroradiologists with three years and eight years of experience in otoradiology independently evaluated depiction of 30 anatomical structures in both the flat-panel CT and MDCT of the 15 specimens in a randomized order. These anatomical structures of the external, middle, and inner ear were evaluated with a 0 to 2 score: 0 = the structure could not be visualized; 1 = the structure could be identified but was not well-delineated from the surrounding tissues, or some parts of the structures were poorly identified; and 2 = the structure was well-visualized and delineated from the surroundings in all of its parts. Meanwhile, they used an anthropomorphic Rando Alderson phantom (Rando Alderson Research Laboratories, New York City, New York) to estimate the radiation dose.
Clear results
While MDCT yielded higher signal, lower noise, higher signal-to-noise ratio (SNR), and fewer artifacts, flat-panel CT showed a significantly higher image quality overall score compared with MDCT (p < 0.0017 after application of the Bonferroni correction for multiple testing). Specifically, FPCT provided better images of 10 structures: the bone marrow of the malleus, the incudomalleolar joint, the anterior crus of the stapes, the posterior crus of the stapes, the footplate of the stapes, the tendon of the tensor tympani muscle, the stapedius muscle, the lateral ligament of the malleus, the modiolus, and the greater petrosal nerve (all p < 0.0017 after application of the Bonferroni correction for multiple testing). Furthermore, no structure was depicted better with MDCT than with flat-panel CT.
In terms of dose, in the current study, flat-panel CT yielded different effective doses to specific organs than MDCT. For example, flat-panel CT had a lower equivalent dose for the thyroid, eye lenses, and salivary glands but higher for the brain, pituitary gland, and bone surface compared with MDCT. The researchers suggested these differences were due to the different x-ray emitter trajectories of the two techniques. Conversely, overall effective doses were similar.
The authors stated there were some limitations to the study: The assessment of specimens could not be blinded because of features such as slice thickness. Furthermore, the use of specimens may have raised the overall image quality for both techniques, but proportionately more for flat-panel CT than MDCT, due to the reduction of scattering artifacts, they noted.
Nevertheless, given their experience with an angiographic C-arm unit for temporal bone FPCT examinations over the past two years, the authors believe the results of the current study largely reflect clinical practice and that flat-panel CT provides higher overall image quality for assessment of the temporal bone compared with a 128-slice CT scanner, with better delineation of 10 anatomical structures and with a comparable radiation dose.
Future work
While the results are significant, further studies should demonstrate if the higher image quality of FPCT provides a diagnostic advantage compared with MDCT for more accurately detecting pathologies such as otosclerosis, for example, according to Conte.
"It is well-known that better image quality does not always provide greater diagnostic accuracy. As an expert in otoradiology, however, my feeling is the diagnostic gain is consistent for most of the indications. Now, given the low dose of both FPCT and new-generation MDCT, researchers could conduct a within-subject analysis in prospective studies, overcoming ethical problems related to the fact that each subject should undergo both examinations," he noted.
The study is a welcome boost for flat-panel CT temporal bone assessment, according to Conte, who noted that some radiologists believe the technique requires dedicated CT scanners, when in fact it can also be performed with angiographic C-arm units equipped with a flat-panel detector, available in many neuroradiology departments, and this without the additional cost of dedicated scanners. He hopes that more radiologists now will be aware of the possibility of using their existing flat-panel angiography systems to perform flat-panel CT of the temporal bone.
While Conte notes flat-panel CT is the gold standard for temporal bone assessment due to its high spatial resolution for studying bony structures with small and complex components, he underlines that because it does not have a high contrast-resolution the unit's neuroradiologists prefer MDCT for obtaining more information about soft tissue, and after contrast agent administration, such as in the case of malignant external otitis. Beyond flat-panel CT's decreased soft-tissue contrast resolution, he also pointed to the technique's increase in scattering artifacts. Furthermore, for less cooperative patients, MDCT offered the possibility of reducing scan time at the expense of spatial resolution.
However, because of flat-panel CT's lower susceptibility to metallic artifacts, the group is now using the technique to study cochlear implants.
"We are trying to provide audiologists information that can be useful both in the surgical positioning of cochlear implants and in postsurgical mapping, ensuring a better outcome to patients," he said.