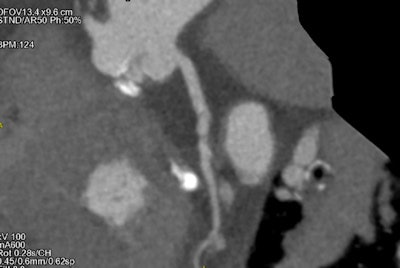
The latest generation of CT scanners can provide excellent images of the coronary arteries, aortic annulus, and aortoiliac anatomy at a low contrast volume and a low radiation dose, even in patients with an irregular heartbeat or a high heart rate, according to new research from Turin, Italy.
"Advances in our knowledge of cardiovascular diseases coupled with technological innovations have enabled the increased use of minimally invasive cardiovascular surgical approaches and transcatheter interventions, with resultant reduced morbidity and hospital stay," noted Dr. Stefano Fiore and colleagues from Turin University Hospital, who presented their findings at the recent European Society of Cardiovascular Radiology (ESCR) congress in Milan.
During minimally invasive and transcatheter procedures, preoperative findings cannot be confirmed by direct visualization of the structures, so imaging plays an increasingly important role in the preprocedural evaluation of patients and for periprocedural imaging guidance, they explained.
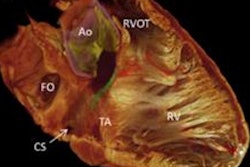
 A 3D reconstruction of the whole aorta of a patient with atrial fibrillation. All images courtesy of Dr. Stefano Fiore, University Radiology Department, A.O.U. Citta della Salute e della Scienza di Torino, Molinette Hospital, Professor Paolo Fonio.
A 3D reconstruction of the whole aorta of a patient with atrial fibrillation. All images courtesy of Dr. Stefano Fiore, University Radiology Department, A.O.U. Citta della Salute e della Scienza di Torino, Molinette Hospital, Professor Paolo Fonio.Study details uncovered
The group conducted a retrospective study to evaluate the effectiveness of a 256-slice CT scanner prior to mitral and aortic valve surgery in the evaluation of the aortoiliac femoral axis and coronary arteries. Their sample consisted of the first 64 consecutive patients (74.2 ± 17.2 years; 33 women, 31 men) scheduled for mitral. The patients underwent CT with a 256-slice-CT system (Revolution CT, GE Healthcare), the exclusion criteria being contraindications to contrast agents and impaired renal function.
Before the CT examination, all patients were informed about the possible use of their data for study purposes, and patients' information was anonymized prior to the analysis. Contrast agent was administered according to the patient's body mass index and glomerular filtration rate, and no premedication for heart rate control was administered. When performed, the invasive coronary angiography served as a reference standard, and the radiologists evaluated images for the presence of 50% stenosis, Fiore and colleagues continued.
The researchers conducted axial prospective assessment (cardiac cycle phases 40% to 80%). ECG-gated scanning was utilized to examine the thorax, and spiral non-ECG-gated scanning of the abdomen immediately followed. The contrast flow was 5 mL per second, followed by 50 mL physiological solution and use of iterative reconstruction (adaptive statistical iterative reconstruction, ASIR-V at 50%). Two experienced radiologists and one resident radiologist performed the analysis.
The key findings
The average volume of contrast media was 55 ± 8 mL, while the average attenuation of all vessels was greater than 350 HU.
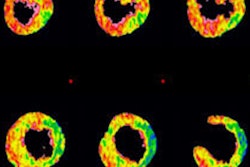
 Reconstruction of the coronary arteries in a patient with atrial fibrillation.
Reconstruction of the coronary arteries in a patient with atrial fibrillation.The evaluation of the peripheral access vessels and dimensions of the ascending aorta, aortic root, and aortic annulus (when requested) were performed in all patients. The mean cardiac frequency was 74.18 ± 12.32 bpm, and the presence of atrial fibrillation in six patients did not affect the diagnostic performance, Fiore and colleagues noted.
Dose length product was 532.3 ± 200.0 mGy-cm, and CT dose index for the axial acquisition was 13.87 ± 6.92 mGy and for the helical 3.85 ± 1.35 mGy.
The authors compared the coronary arteries in a CT angiography examination and an invasive coronary angiography exam by studying four vessels: the left coronary artery common trunk, left coronary artery anterior descending branch, circumflex artery, and right coronary artery. Ten vessels were not assessable in the CT angiography examination because of artifacts due to the presence of widespread calcifications or patient movement artifacts.
In 39 patients, the coronary CT angiography was negative, and subsequently no other exams were performed. In the other 21 cases, invasive coronary angiographies were performed, and on a per-patient analysis, CT achieved a diagnostic accuracy of 79.8%.
The scientific posters from the ESCR 2017 meeting are available in the European Society of Radiology's EPOS database. To view the exhibit and clinical images by Fiore and colleagues, click here.