The addition of category 4X lesions in the Lung CT Screening Reporting and Data System (Lung-RADS) imaging scheme adds value and increases malignancy yields among experienced radiologists, according to a Dutch study in Radiology. The 4X nodules turn out to be malignant in half of cases.
To test the utility of the new 4X (highly suspicious for malignancy) classification for increasing the diagnostic yield for lung cancer, researchers analyzed nearly 400 subsolid nodules (SSNs) from the National Lung Screening Trial (NLST) that would have been classified as Lung-RADS category 3 or higher. Experienced chest radiologists determined which nodules to upgrade to category 4X, and malignancy rates were then compared with purely size-based categories. The malignancy rate for 4X nodules was substantially higher than the malignancy rates for category 3, 4A, and 4B SSNs, the group found.
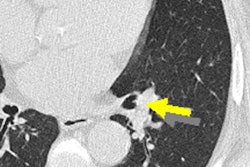
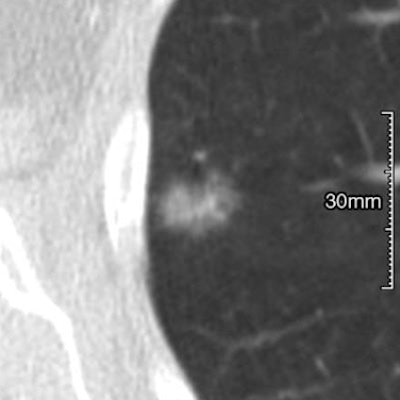
 CT scans of subsolid nodules for which upgrade to category 4X was determined variably by the six observers. (a, left) Malignant lesion upgraded by three observers. (b, middle) Malignant lesion upgraded by four observers. (c, right) Benign lesion upgraded by two observers. Images republished with permission of RSNA from Chung et al, Radiology, March 24, 2017.
CT scans of subsolid nodules for which upgrade to category 4X was determined variably by the six observers. (a, left) Malignant lesion upgraded by three observers. (b, middle) Malignant lesion upgraded by four observers. (c, right) Benign lesion upgraded by two observers. Images republished with permission of RSNA from Chung et al, Radiology, March 24, 2017."Our results indicate that the application of category 4X for suspicious SSNs is of substantial added value in the Lung-RADS system, with very high malignancy rates in the hands of experienced radiologists," wrote study authors Dr. Kaman Chung, Dr. Cornelia Schaefer-Prokop, PhD, and colleagues from Radboud University Medical Center in Nijmegen, the Netherlands.
Difficult read
Differentiating SSNs plays an important role in predicting their malignancy; however, studies have shown high variability among radiologists in classifying nodules as subsolid, often due to disagreement on the presence or size of a solid component at CT imaging. SSNs often manifest as early adenocarcinomas, with the size of the solid component correlating with the histological characteristics of invasive adenocarcinomas.
Hoping to better characterize the malignancy risk of these nodules, Lung-RADS recently introduced category 4X for lesions that demonstrate "additional findings that increase the suspicion of malignancy," even though the precise criteria for designating a category 4X lesion morphologically are still evolving. Assignment of this category, reserved for category 3, 4A, or 4B nodules, triggers a more intensive diagnostic workup than nodule size alone would otherwise indicate.
Yet the degree to which the addition of category 4X actually improves Lung-RADS' performance for predicting the probability of malignancy is poorly understood. This study aimed to "evaluate the added value of Lung-RADS category 4X over categories 3, 4A, and 4B in the differentiation between benign and malignant SSNs," Chung and colleagues wrote (Radiology, 24 March 2017).
In their study, the researchers identified SSNs on all baseline CT scans from the NLST that would have been classified as Lung-RADS category 3 or higher, totaling 374 SSNs for analysis. An experienced screening radiologist segmented all of the nodules and located all malignant SSNs that could be seen on baseline CT scans.
From there, six experienced chest radiologists independently determined which nodules to upgrade to category 4X, denoting a higher risk of malignancy. They compared the malignancy rates of purely size-based categories with those assigned to Lung-RADS category 4X, and made a similar comparison of false-positive rates between size-based nodules and category 4X lesions. Fleiss' kappa statistics were used to calculate observer variability.
More cancers
In all, 15% to 24% of the SSNs were upgraded to category 4X, and these nodules had malignancy rates of 46% to 57%, depending on the observer. These rates were substantially higher than those of category 3, 4A, and 4B SSNs without observer intervention, the authors reported.
"The results of our study therefore indicate that the inclusion of a 4X category for suspicious lesions in a nodule management tool provides substantial added value and results in high malignancy rates in category 4X SSNs," they wrote.
| Malignancy rates of nodules by observer | ||||
| Lung-RADS category | ||||
| 3 | 4A | 4B | 4X | |
| Observer 1 | 5% | 16% | 10% | 52% |
| Observer 2 | 2% | 7% | 9% | 57% |
| Observer 3 | 4% | 10% | 11% | 55% |
| Observer 4 | 5% | 14% | 13% | 53% |
| Observer 5 | 4% | 7% | 7% | 46% |
| Observer 6 | 5% | 8% | 10% | 53% |
| Average | 4% | 10% | 10% | 53% |
The observers were also asked to specify morphological features, but only for nodules assigned to category 4X.
"Therefore, we cannot draw conclusions as to whether these morphologic features enable differentiation between benign and malignant lesions; rather, the fact that almost no significant differences in morphologic criteria were seen between true- and false-positive 4X lesions emphasizes the overlap of certain morphologic features if visually assessed," they wrote.
In addition, the agreement among radiologists as to which SSNs should be upgraded was only moderate, underlining the subjectivity of the selection process.
| Characteristics considered suspicious for malignancy | ||
| Average No. of findings among readers | 95% confidence interval | |
| Internal structure | 44 | 28-59 |
| Border characteristics | 43 | 28-58 |
| Solid core characteristics | 19 | 5-32 |
| Effect on surrounding tissues | 23 | 15-31 |
| Effect on bullae | 20 | 10-29 |
The readers successfully increased the malignancy rate in category 4X to about 50%, but they used different morphological criteria to choose their cases, according to the authors.
"This suggests that it may be difficult to establish suspicious morphologic features," they wrote. No features revealed a statistically significant difference by all six observers between falsely upgraded benign and correctly upgraded malignant 4X lesions.
The highest malignancy rate among the size-based categories was for 4B lesions, at 10%, compared with an estimated malignancy rate of more than 15% for Lung-RADS 4B. For the other categories, Lung-RADS malignancy rates were generally in line with study findings.
The results also showed that a subjective, purely visual scheme such as Lung-RADS resulted in an upgrade of benign lesions that would have unnecessarily undergone more intense workup, including biopsy or resection. Among the falsely upgraded lesions, 27% were transient, which is proof of the transient character of category 4X lesions. Short-term follow-up could avoid unnecessary invasive management, the group wrote.
Short-term follow-up is key
Absent significant identifying morphological features, Fleischner Society guidelines recommending short-term (three-month) follow-up of lesions seem to be the most useful approach for avoiding unnecessary intervention, according to Chung and colleagues.
Among the study's limitations, readers were not asked to follow the entire Lung-RADS protocol. Also, morphologic features were scored only in upgraded lesions, precluding multivariate analysis of benign and malignant nodules by morphological characteristics. Finally, the readers were all experienced but without specific training, further underlining the subjective nature of 4X categorization, the authors wrote.
"The addition of category 4X for suspicious subsolid nodules is of substantial value in [Lung-RADS] and has high malignancy rates of 46% to 57% in the hands of experienced radiologists," they concluded.