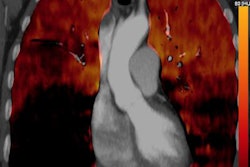
Adding lung and venous ultrasound into the diagnostic process for pulmonary embolism (PE) can yield improved sensitivity and specificity, obviating the need for CT pulmonary angiography in many cases, according to research from Italy that will be published in the March issue of Academic Emergency Medicine.
In a multicenter study involving more than 400 patients, an Italian research team found that combining lung and venous ultrasound, Wells score, and D-dimer test results would have avoided the need to perform CT pulmonary angiography (CTPA) in half of cases with suspected PE. In comparison, a traditional approach based only on the Wells score would have bypassed CTPA in just over 25% of the patients, concluded the team led by Dr. Peiman Nazerian from Careggi University Hospital in Florence.
As a result, a diagnostic strategy that integrates clinical information, lung and venous ultrasound, and D-dimer results "may increase the performance of risk stratification and may reduce the use of CTPA in the diagnostic approach to PE, [while] still maintaining an acceptable safety profile," the authors wrote.
Improving PE prediction?
In cases of suspected pulmonary embolism, international guidelines currently recommend combining plasma D-dimer test results with clinical scoring systems such as the Wells score to optimize the diagnostic process and the use of CTPA for final confirmation, according to the group. Point-of-care ultrasound is increasingly being used, though, for assessing acute patients, including conditions such as dyspnea, chest pain, syncope, and shock in which PE is the differential diagnosis. Recent studies in the literature have also assessed the diagnostic performance of ultrasound in patients with suspected PE, according to the authors.
"However, apart from the intrinsic diagnostic power of ultrasound in the definitive diagnosis of a complex disease, to date no one investigated the possibility of improving the prediction rules for PE by integrating clinical data with lung and venous ultrasound," they wrote.
As a result, the researchers sought to compare the diagnostic performance of the Wells score with a model that combined the score with lung and venous ultrasound findings. They also wanted to determine if CTPA utilization could be reduced by a diagnostic strategy based on both clinical and ultrasound data.
To conduct an observational multicenter study of diagnostic accuracy, Nazerian and colleagues recruited adult patients suspected of having PE from four Italian university hospital emergency departments between July 2014 and April 2015. After an attending physician established a suspicion of PE and adjudicated items in the Wells score, one of 20 sonographer investigators performed lung and venous ultrasound.
The investigators included eight senior physicians (seven internal medicine specialists and one pulmonologist) as well as 12 internal medicine, emergency medicine, or pulmonology residents with six months of practical experience in producing their own lung and venous ultrasound exams. All participants were blinded to diagnostic tests and to all clinical information, with the exception of presentation and visible signs.
Ultrasound-enhanced Wells score
Using predefined ultrasound protocols, the studies were performed on one of 11 ultrasound scanners, including three MyLab Gold, one MyLab 40, one MyLab 50, and one MyLab Alpha (Esaote); one Logiq 3 and one Logic 5 Pro (GE Healthcare); and one HD7 (Philips Healthcare). Two items of the Wells score were then recalculated based on the ultrasound signs detected by the sonographer: "Signs and symptoms of DVT" was replaced by "venous ultrasound positive for DVT," and "alternative diagnosis less likely PE" was replaced by "alternative diagnosis less likely than PE after lung ultrasound."
If at least one pulmonary infarct was seen on lung ultrasound, the "alternative diagnosis less likely than PE after lung ultrasound" item was considered positive and assigned a score of three points. Zero points were given if there were no infarcts and if a condition of sonographic findings compatible with an alternative pulmonary diagnosis was detected. For both the traditional Wells score and the modified Wells score enhanced by ultrasound findings, a diagnosis of PE was considered unlikely for scores of 4 or less.
Blinded to the ultrasound results, the attending physician ordered a multidetector CTPA or lung scintigraphy exam in accordance with the standard of care. Of the 446 patients included in the final research study, 297 (66.6%) received a CTPA exam, while nine (2%) had a scintigraphy exam. Pulmonary embolism was confirmed in 125 (28%) patients.
| Wells score + ultrasound for diagnosing PE | ||
| Conventional Wells score | Wells score enhanced by ultrasound findings | |
| Sensitivity | 57.6% | 69.6% |
| Specificity | 68.2% | 88.2% |
In combination with D-dimer results, a Wells score enhanced by the ultrasound findings had a failure (false-negative) rate of 0.8% when used in a diagnostic strategy to rule out PE. It also offered an efficiency rate (the proportion of patients with a negative D-dimer result combined with a Wells score that indicated PE was unlikely) of 32.3%, slightly higher than the 27.2% efficiency rate produced by a diagnostic strategy using the conventional Wells score.
Importantly, further analysis showed that a strategy based on lung and venous ultrasound with D-dimer would enable 50.5% of patients to avoid CTPA, compared with 27.2% of patients when the rule without ultrasound is applied.
Here to stay?
The research findings suggest that lung ultrasound can show alternative diagnoses such as pneumonia or pleural effusion, according to a statement from the Society for Academic Emergency Medicine (SAEM). These results, along with a 2015 meta-analysis in PLOS One that found lung ultrasound yielded useful overall diagnostic accuracy, suggest that lung ultrasound is here to stay and should be considered when evaluating patients with suspected PE, the society said.
The widely used Wells score is often criticized for the vagary surrounding the definition of its "alternative diagnosis more likely than PE" term, noted Academic Emergency Medicine Editor-in-Chief Dr. Jeffrey Kline.
"Most clinicians who believe an alternative diagnosis is more likely than PE cannot name the diagnosis," Kline said in the SAEM statement. "Nazerian et al show that lung ultrasound can quickly and noninvasively allow physicians to literally see the identity of 'something else wrong' other than blood clots in the lung. This advantage can help them be more confident in deciding not to order expensive testing that causes large doses of radiation exposure to patients."