PET/MRI's efficacy in women's imaging applications continues to broaden. Now German researchers have found the hybrid modality achieves "superior restaging" with breast cancer patients compared with MRI alone in a study published online on 23 January in the European Journal of Radiology.
There were, however, a couple of caveats to PET/MRI's performance. The inclusion of MRI sequences, such as diffusion-weighted imaging (DWI), can extend scanning time with debatably beneficial results, researchers from the University Hospital Essen concluded.
"Our results endorse this data in revealing the excellent diagnostic accuracy as well as superior diagnostic confidence of PET/MRI for the identification of recurrent breast cancer lesions, with significantly higher values if compared to MRI alone," noted lead author Dr. Johannes Grueneisen.
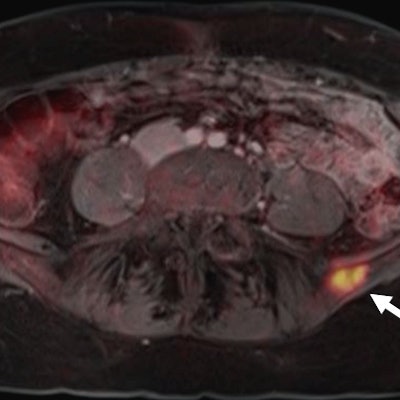
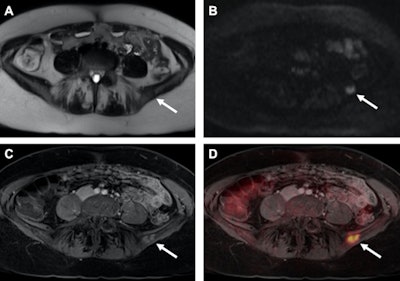 Images of a patient with recurrent breast cancer and a PET-positive bone metastasis of the left iliac wing, which can be identified on T2-weighted HASTE (A) as well as on DWI (B, arrows). The identical tumor lesion shows moderate contrast-enhancement on T1-weighted VIBE images (C) and can be detected with a higher conspicuity after image fusion on PET/MRI (D). All images courtesy of Dr. Johannes Grueneisen.
Images of a patient with recurrent breast cancer and a PET-positive bone metastasis of the left iliac wing, which can be identified on T2-weighted HASTE (A) as well as on DWI (B, arrows). The identical tumor lesion shows moderate contrast-enhancement on T1-weighted VIBE images (C) and can be detected with a higher conspicuity after image fusion on PET/MRI (D). All images courtesy of Dr. Johannes Grueneisen.PET/MRI utilization
PET/CT became the standard hybrid imaging option for staging and restaging breast cancer soon after the modality's introduction almost 20 years ago. Accurate evaluation of the disease is particularly critical in order to choose the most appropriate treatment strategy and improve a patient's prognosis, both of which are limited in cases of breast cancer recurrence.
With the relatively recent advent of PET/MRI, the "successful integration of the PET component within an MR-scanner provides a new generation of multimodal imaging, combining functional PET data with structural and functional information of MRI," the authors wrote.
 Dr. Johannes Grueneisen from University Hospital Essen.
Dr. Johannes Grueneisen from University Hospital Essen.Grueneisen and colleagues have been quite proficient in recent years investigating the utility of PET/MRI for women's imaging. At RSNA 2016, the Essen group presented a study, which found PET/MRI was a valuable tool in accurately staging tumors of the uterine cervix and may serve as an alternative modality for a clinical workup prior to treatment.
A 2015 study by Grueneisen et al. found that PET/MRI achieved high diagnostic performance for restaging gynecological cancer patients compared with FDG-PET/CT, with only a slightly longer scan time and "markedly reduced" radiation exposure. In 2014, the German researchers concluded that adding DWI to FDG-PET/MRI to stage women with primary or recurrent pelvic malignancies contributed minimal value and is not worth the additional scan time.
In the current EJR study, Grueneisen and colleagues noted that "well-defined and efficient" MRI protocols were needed to achieve high diagnostic results and to overcome "prolonged examination times, mainly caused by the acquisition of a substantial number of different MR sequences, resulting in potential patient discomfort."
Imaging protocols
The researchers prospectively evaluated 36 consecutive female patients with a mean age of 58 (± 14 years, range of 28-78 years) with a suspected recurrence of breast cancer. Subjects initially had undergone treatment after their first diagnosis of breast cancer and were considered free of the disease for at least six months prior to PET/CT and PET/MRI.
The women first received a whole-body PET/CT scan (Biograph mCT 128, Siemens Healthineers), with FDG administered 60 minutes before imaging. Contrast-enhanced (Ultravist 300, Bayer HealthCare) CT also was performed as part of the procedure.
The whole-body PET/MRI scan was conducted in the supine position using a 3-tesla MRI (Biograph mMR, Siemens Healthineers), with imaging starting an average of 133 minutes (± 25 minutes) after FDG injection. The MRI protocol included the following:
- T2-weighted half-Fourier acquisition single-shot turbo spin-echo (HASTE) with DWI
- HASTE with T1-weighted volumetric interpolated breath-hold examination (VIBE)
- A combination of HASTE, DWI, and VIBE
Two readers identified tumor relapses in both MR and PET/MRI readings two weeks apart to avoid recognition bias. Lesion conspicuity also was evaluated on a 4-point scale for the three different MRI sequences.
Lesion discoveries
Based on the reference standard of histopathological samples, the researchers discovered tumor recurrence in 25 (69%) of the 36 patients. MRI alone correctly identified 22 (88%) of the 25 relapsing tumors, with a true negative in 10 (91%) of the remaining 11 tumors. In comparing the results of MRI alone and PET/MRI, there was no statistically significant difference (p > 0.05).
| MRI vs. PET/MRI | ||
| MRI alone | PET/MRI* | |
| Sensitivity | 88% | 96% |
| Specificity | 91% | 91% |
| Positive predictive value | 96% | 96% |
| Negative predictive value | 77% | 91% |
| Accuracy | 89% | 94% |
In addition, the scans revealed a total of 165 suspect lesions, of which there were 122 malignant tumors (74%) and and 43 benign lesions (26%). Among the 25 patients with breast cancer relapse, 18 patients (72%) experienced metastatic disease. The other seven patients (28%) suffered from unifocal cancer localizations, and a local breast cancer recurrence was found in five patients (20%).
In the comparison of the modalities, PET/MRI and the three MR imaging sequences were significantly better than MRI alone.
| Comparison of modalities | ||||
| MRI alone | PET/MRI* | |||
| HASTE/DWI | HASTE/VIBE | HASTE/DWI/VIBE | ||
| Sensitivity | 82% | 93% | 94% | 95% |
| Specificity | 86% | 91% | 91% | 93% |
| Positive predictive value | 94% | 97% | 97% | 98% |
| Negative predictive value | 63% | 81% | 85% | 87% |
| Accuracy | 83% | 92% | 93% | 95% |
Regarding lesion conspicuity and differentiating between malignant and benign lesions, contrast-enhanced T1-weighted VIBE imaging performed the best with significantly higher values compared with T2-weighted HASTE or DWI. T2-weighted HASTE also outperformed DWI in distinguishing benign lesions, while there was no statistically significant difference between the two MR sequences in differentiating malignant lesions (p > 0.05).
Scan times
In addressing the issue of scan time, PET/MRI exams took approximately 27 minutes (± 4 minutes). By excluding a postcontrast T1-weighted VIBE sequence and related activities, the researchers estimated total scan time could be reduced to 25 minutes (± 2 minutes). By skipping the DWI sequence, scan time could decline even more significantly to 19 minutes (± 1 minute).
Given the need to optimize dedicated MRI scan protocols for efficient whole-body PET/MRI for oncology, the results "support the application of fast, yet morphologically adequate PET/MR protocols," Grueneisen and colleagues wrote. "Accordingly, considering an equivalent accuracy for the detection of breast cancer recurrences in the three PET/MR readings, the application of contrast agent and the inclusion of DWI in the study protocol seems to be debatable."