A sound knowledge of clinical details, including tumor markers, is vital when interpreting gynecologic images, because this information enables the radiologist to make an accurate diagnosis, according to award-winning researchers from a top London teaching hospital.
This point is only one of many made by Dr. Saranya Vickramarajah from the gynecology oncology tumor board at Imperial College and colleagues in an e-poster presentation that received a certificate of merit at RSNA 2016.
"Gynecology cases often involve multimodality imaging, which can be complex," they noted. "The tumor board environment provides the opportunity to review imaging with clinical detail and tumor markers, which are frequently not available to the reporting radiologist. This often provides important learning opportunities."
Key points to remember
To help radiologists improve their diagnostic accuracy, Vickramarajah and colleagues emphasized the following four points:
- Awareness of benign conditions that may mimic malignancy is essential, and it is important to be aware of the radiological features that can differentiate them, because clinical management is often significantly altered.
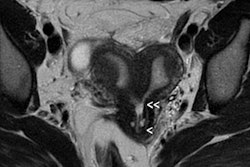
- It is imperative to correctly stage tumors and recognize when disease is no longer resectable so that the correct treatment algorithm can be used.
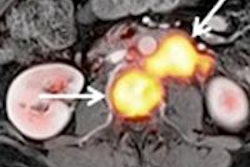
- It is important to recognize the primary tumor may not be gynecologic in origin, and other tumors can involve the female reproductive tract.
- Fibroids remain a diagnostic challenge, benign disease can take on a highly varied appearance, and malignancy has no pathognomonic features. An enlarging fibroid in the postmenopausal age group should always be treated with caution.
The researchers have other pearls of wisdom to share. For instance, tuberculosis should be considered when there is diffuse peritoneal disease, and tumor markers, such as CA-125, may be raised but often not to the same extent as seen with ovarian cancer.
"It is critical to make the diagnosis, as the treatment options are drastically different," they added. For instance, tuberculosis is treated with antibiotics; ovarian cancer is treated with surgery or chemotherapy. Tumors can metastasize to the ovaries, and bilateral ovarian tumors may represent stage II ovarian cancer, but they may also be metastatic. The surgical treatment options for different cancers are not the same, so diagnosing the primary lesion is important.
Peritoneal abnormalities
When it comes to peritoneal abnormalities, they are not always secondary to malignancy, Vickramarajah and colleagues continued.
"The reading radiologist should be aware of the many possible benign etiologies: infective, inflammatory, and secondary to chronic disease," they stated. "CA-125 is a nonspecific marker, and levels are raised in many causes of peritoneal irritation. However, in these situations, CA-125 is often not grossly elevated."
The group also urges radiologists to be aware that other malignancies may mimic gynecological malignancy.
"It is important to know the patient's past medical history, particularly if there is a history of malignancy, and also to carefully review the other abdominopelvic organs," they explained.
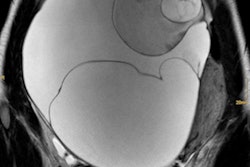
Also, do not misdiagnose a dilated fallopian tube as a cystic ovarian mass, they cautioned.
"The reading radiologist should be aware that a complex adnexal mass is not always ovarian in origin," they emphasized. "Look for features that suggest a dilated tube -- 'S-' and 'C-'shaped tubular regions, incomplete septations when cut axially, [and] mucosal folds when partially distended."
Finally, radiologists should also be aware of imaging features that allow a confident diagnosis of benign disease.
"In benign disease, it may be possible to delineate normal ovarian stroma, a feature which is reassuring but should not always be taken to indicate benignity," they said. And be aware that malignant transformation can occur on the background of benign disease.