Breast cancer remains the most common cause of cancer-related death for women in western countries, but Dr. Christiane Kuhl is convinced MRI screening can bring about major changes. In this interview, Kuhl, a professor of radiology and the director of the Department of Diagnostic and Interventional Radiology at the University of Aachen in Germany, speaks about her group's current areas of research and the future challenges.
German Radiological Society (DRG): You gave a presentation at the 2016 German Radiology Congress about "Breast cancer in 2020 -- what is the future of radiology?" Can you tell us about your research?
Kuhl: Breast cancer diagnosis, especially using MRI, is diversifying. Our research focuses on two main things. On the one hand, we're developing more complex imaging methods to keep pace with the sharply rising demand for imaging biomarkers for precision medicine, and on the other, we're slimming down previously complicated techniques to create what we call abbreviated breast MRI.
 Dr. Christiane Kuhl.
Dr. Christiane Kuhl.What exactly do you mean by precision medicine?
Precision medicine uses targeted therapies, i.e., treatments which focus on very specific and clearly defined features of cancer cells. One well-known example is anti-hormone treatment of receptor-positive breast carcinomas, or Herceptin (trastuzumab) for Her2-enriched cancers. However, a carcinoma is already categorized as receptor positive if just over 10% of its cells have these receptors. Contrary to previous opinion, tumors are heterogeneous, made up of different types of cells. Plus, they can change over the course of therapy and develop resistance just as bacteria do against antibiotics. Therefore, we need new examination techniques that can identify these properties, find possible docking sites for new cancer treatments, and discover any resistance to targeted therapy at an early stage.
So we're planning to develop an MR surface coil with an integrated, fully digital PET detector as part of the EU-funded Horizon2020 project. This will pursue a completely new approach to hybrid PET/MR imaging -- by integrating PET detectors into a radiofrequency coil, we will be able to turn any regular MR system into a high-resolution MR-PET hybrid scanner.
What is abbreviated MRI technology?
Our second area of research is working in completely the opposite direction, by simplifying an often complex procedure. We launched the abbreviated MRI concept two years ago.
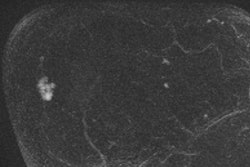
An MR examination normally consists of many different parts, i.e., pulse sequences. The principle of abbreviated MRI is to identify those parts of the MR scan that give us the most important information about a particular issue, and then home in on them. For example, we carried out a large-scale prospective study showing that you can detect early breast cancer using abbreviated MRI within a scan time of just three minutes. More importantly, an experienced breast radiologist can use these scans to rule out breast cancer in just three seconds.
Abbreviated MRI was also perfectly feasible as an early detection method on a larger scale. The international response to this study has been overwhelming.
But isn't MRI screening as part of comprehensive breast cancer prevention too expensive?
In its traditional form, definitely, but abbreviated MRI will very significantly cut examination costs. This will work even better once we have MRI scanners optimized for high-volume early breast cancer detection and some manufacturers are already rising to the challenge. Because our method is the first to use larger or even full-scale MRI for the early detection of breast cancer, it has stirred up great interest. Pilot projects based on ours are being launched in the U.S., China, and various European countries. In the U.S., a large-scale multicenter study (Abbreviated Breast MRI Trial -- EA1141) funded by the ECOG-ACRIN Cancer Research Group is being conducted, where Dr. Christopher Comstock from Memorial Sloan Kettering Cancer Center, Dr. Gillian Newstead from the University of Chicago, and myself serve as principal investigators.
Just three minutes of MRI and an equally short time for the radiology diagnosis -- is that enough?
Absolutely. And this was with no significant loss of accuracy or diagnostic reliability. Most importantly, it allowed much better early detection than mammography. We're detecting breast cancer much earlier and more reliably.
Why is early detection MRI better than other methods?
There are two different issues. Firstly, it's clear that MRI is identifying breast cancer more reliably and accurately than any other method; it's around three times as reliable as digital mammography, and twice as good as combined mammography and ultrasound. But it's equally important to know which carcinomas are found using which methods. The term "breast cancer" refers to a heterogeneous group of diseases with very different prognoses. We've found that MRI is especially good at detecting the very fast-growing, aggressive carcinomas, which is something mammography is very bad at.
Don't mammograms show up aggressive tumors?
They're less reliable. On a mammogram, aggressive, fast-growing carcinomas can look like benign tumors or even normal breast tissue, which means they may get diagnosed too late. But they show up very well on MRI exams because the processes that maintain the growth of the cancer and keep it supplied with blood and nutrients make it "light up" on the MRI.
And which carcinomas is mammography good at detecting?
Mammograms depict regressive changes, such as calcifications and architectural distortions, both secondary to hypoxia and cell death. This is why mammograms tend to detect slow-growing, less aggressive tumors and ductal carcinoma in situ (DCIS). We've known for a long time that breast cancers that are detectable by mammography have a better prognosis than those that aren't -- this is known as "length-time bias." We also know that some even aren't worth treating because the patient can't expect any benefit -- a situation referred to as "overdiagnosis" and "overtreatment."
Do you need a contrast medium for these MRI exams?
It doesn’t work without contrast, because that’s the only way of highlighting cancer-related alterations such as angiogenesis and protease activity. I do not think that this is a major impediment because MRI contrast agents are very well tolerated. It’s recently been shown that multiple intravenous injections of contrast agents may lead to bright signal in specific areas of the brain due to traces of gadolinium. This does not cause clinical symptoms. We can see them on brain MRI only because they are meant to cause T1-shorterning, i.e., act as contrast agent. If other medication or nutrients we ingest caused the same strong T1 shortening we would probably be surprised to see how much stuff accumulates in the brain.
When you’re weighing up these theoretical risks, it’s important to remember that unlike mammography, MRI doesn’t use radiation.
So, do you want your MRI approach to replace mammography as the screening method?
It's certainly time to think about better early detection. MRI is still the most complex and expensive breast examination method, but it's also by far the most effective. This is now accepted worldwide, but it's still a challenge to make this complex method more widely available. And abbreviated MRI could be the procedure that marks a turning point.
You think the screening program as it stands is no longer adequate?
We’ve clearly benefited from the introduction of screening mammography, because it gives us a quality-assured early screening for the general population. It will still be a long time before abbreviated MRI is available for screening, if ever at all. Breast MRI is not even sufficiently available for diagnostic breast MRI purposes. If you compare this with other conditions that are much less important such as tennis elbow or meniscus degeneration -- conditions that are consistently examined by MRI, and yet it’s not even available to women to plan breast cancer treatment. I find this difficult to comprehend.
What specific improvements do you expect to result from MRI breast-cancer screening?
Mammography has been used for decades in many countries, but the basic problem hasn't really changed: breast cancer is still the most common cause of cancer-related death for women in Western countries. MRI screening could finally bring about major changes to this.
Editor's note: This is an edited version of a translation of an article published in German online by the German Radiological Society (DRG, Deutsche Röntgengesellschaft e.V.). Translation by Syntacta Translation & Interpreting. To read the original article, published to coincide with the International Day of Radiology, click here.