
In the aftermath of the gun attacks and bombings in Paris on 13 November, management and staff in key hospitals across the city met internally to identify areas of procedure that worked and where improvement was needed in the event of another wide-scale terror strike. Present at those meetings were the radiologists interviewed by AuntMinnieEurope.com, with their views on how services coped during the crisis and how departments can prepare for any future attacks.
Dr. Yves Menu, a member of the board of directors at Saint-Antoine Hospital, and a former ECR president, points to several problem areas in the emergency procedures known as "the White Plan" (Plan Blanc) that have been addressed in recent months.
"There was no specific room for the psych team to use in the initial hours when trying to work with the victims' families, no suitable room to be used as the crisis 'headquarters', and an out-of-date list of on-call staff, which still contained the names and contact details of people who had left the institution and which lacked those of newly recruited staff," Menu said. "This on-call list also lacked detail about specific competences of medical staff. For example, in radiology the situation might demand a CT or interventional radiology expert and not everybody may be experienced in those subspecialties."
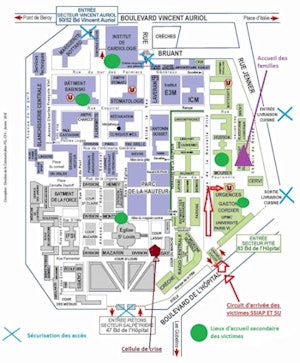
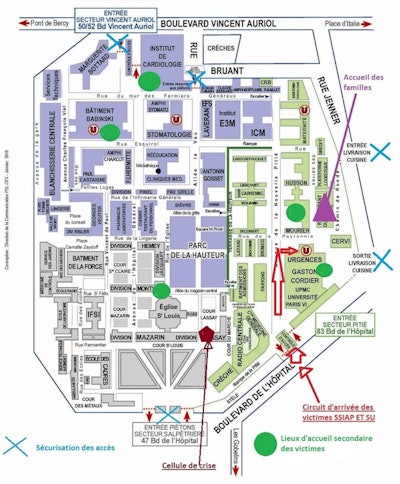
Implementation of the White Plan at Pitié-Salpêtrière hospital. Image courtesy of Dr. Philippe Grenier. Original source: Annales françaises de médecine d'urgence, February 2016, Vol. 6:1, pp. 47-54.
Translation clockwise starting from the top:
Dark blue: Entrée secteur Vincent Auriol -- Entrance to Vincent Auriol sector
Purple: Accueil des familles -- Family reception area
Black: Entrée livraison cuisine -- Kitchen delivery entrance
Black: Sortie livraison cuisine -- Kitchen delivery exit
Green: Entrée secteur Pitié -- Entrance to Pitié sector
Red: Circuit d'arrivée des victimes SSIAP et SU -- Victim arrival route/fire brigade and emergency services
Green circles: Lieux d'accueil secondaire des victimes -- Secondary reception area for victims
Maroon: Cellule de crise -- Crisis headquarters
Gray: Entrée piétons secteur Salpêtrière -- Pedestrian entrance to Salpêtrière sector
Light blue crosses: Sécurisation des accès -- Securing of entrance/exit points
IT was also addressed at the debriefing meetings, but this issue is one that Menu had raised with management before November, as residents had regularly complained about a slowdown in PACS and report transfer between 3 a.m. and 5 a.m.
"Nighttime is scheduled for administrative data transfer because usually the network is less busy with medical problems. However, the consequence is severe alteration of the transfer rate and speed from PACS. We learned that it was important to be able to stop administrative transfers and to bring back the priority to patient care. The IT team at Saint Antoine has now made this feasible. Furthermore, an IT expert will be part of the official on-call team in any similar future emergency."
Decentralized contact strategy
The meetings have also resulted in updated documents and a less centralized organization. Should another crisis occur, administrative staff will contact one of several "managers" in each department. These local managers each have an updated shortlist of department staff and their competences so that whichever manager is available at the time can choose which staff will be most useful in the circumstances depending on their skillset.
 Dr. Yves Menu returned to Paris from a conference in Italy when he heard the news. Image courtesy of the European Society of Radiology (ESR).
Dr. Yves Menu returned to Paris from a conference in Italy when he heard the news. Image courtesy of the European Society of Radiology (ESR).This decentralized "phone tree" means the responsibility of contacting appropriate medics is not just in the hands of administrative personnel who will probably not know which skills are relevant. Furthermore, all department doctors will have the phone numbers of the other department doctors.
Although most staff that came to work on the night of 13 November arrived spontaneously having been contacted by friends and colleagues, Menu said such informal social networks may not always work, and an official contact strategy needs to be in place in every hospital.
In addition, team preparation should not be based on specific specialties but on efficient collaboration with other wards, especially the emergency unit, which played the central organizing role, according to Menu.
All patients have now left the critically ill units and have returned home or to rehabilitation centers. Some will need additional procedures and surgery, and many still need psychological support.
Menu commended the courage and life-saving efforts of hospital staff in his New Year address, and highlighted how a significant number needed counseling and support after the attacks.
"Being able to talk with a psychologist and with other members of the department, feeling that they were highly appreciated, even celebrated, and receiving a small token of financial compensation for the time dedicated to the victims of the attacks have been to some degree, important elements in their recovery," Menu said.
Heightened alert
An increase in on-call radiologists has been discussed at Saint-Antoine. Senior radiologist, Dr. Catherine Phan who was on duty on 13 November and who led the radiology team as events unfolded, believes two senior radiologists and two residents should be the minimum number of duty doctors imaging high patient numbers in such circumstances, which is double the usual numbers for a shift.
She describes tightened security at the hospital since the Paris attacks: all bags are checked at a security point at each entrance. Security guards even check the boots of cars and taxis waiting directly outside the hospital doors. In the event of White Plan implementation, doctors will need to show ID badges to enter the hospital.
A psychological support meeting in the week following the attacks which aimed to prevent grave delayed reaction, allowed staff to express their feelings and learn how anxiety might manifest itself.
 Members of Saint-Antoine's imaging team who worked on 13 and 14 November. Dr. Catherine Phan is shown third from the left.
Members of Saint-Antoine's imaging team who worked on 13 and 14 November. Dr. Catherine Phan is shown third from the left."Although life carries on, it is in the back of everyone's mind that this kind of attack could happen again. Since early January, there has been regular media coverage of events in November and of the possibility of further events. The risk of attack has been elevated several times in the past three months," Phan noted.
Dr. Philippe Grenier, chair and professor of radiology at Pitié-Salpêtrière Hospital, who made his way to the department as soon as he'd heard about the attacks, has also seen changes at his hospital as a direct result of the night's events.
A meeting comprising 60 staff members representing all the specialties involved in patient care on the night of the attacks and into the early hours took place in the second week of January to establish the strengths of weaknesses of protocols in place across the hospital. Here, too, the list of specialized workers to be called was found to be lacking data, particularly in terms of describing specialty and specific skills. Without this vital knowledge, in some cases administration ended up calling staff who did not have the appropriate competences.
"Administration will still be in charge of calling in workers, but they now have an updated list of subspecialties and competences, as well as criteria. For instance, in the case where trauma CT is required for a number of patients, staff now know they shouldn't just call a neuro radiologist, but also a body radiologist," Grenier said. "Furthermore, the updated list contains not just staff mobile numbers, as mobile networks can be subject to sabotage and also are often busy when a big event takes place, but also landlines."
Relief teams
A related improvement is the hospital will now ensure rotation of emergency staff after six hours to limit fatigue. All staff has been organized into two lists that together cover up to eight six-hour shifts over a time frame extending to 48 hours, if necessary. This means in the event of a future attack, a first emergency team will be called to come in and the second emergency team will be informed they may be required after six hours.
As hospital workers are now classified by specialist areas and team, administrative staff will know that if a number of patients are arriving with gunshots to the abdomen for example, they will need to call a gastrointestinal CT expert in the first team. Each list is lengthy to factor in absences on the day.
More than half of the attack victims arriving at the hospital were without formal identity and staff had to work with the families to identify them using photos, jewelry, or mobile phones found on the person. The high number of patients arriving without identification meant Pitié-Salpêtrière ran out of numbers to identify them using its own local code. As corrections to identification started to be made on the hospital system, some patients ended up with duplicated files -- which led to confusion when accessing history and reports and when updating treatment notes.
"Any change of identification or code during a hospital stay can introduce errors," Grenier said. "For future crises, the emergency services (SAMU - Service d'Aide Médicale Urgente) transporting victims to hospital will identify them with a coded bracelet. The hospital server will then create a unique identification number linked to the code provided by SAMU which will remain the reference number for each patient from arrival on the premises and for the duration of hospital stay."
Three patients are still hospitalized at Pitié-Salpêtrière, two of whom are in rehabilitation, while one remains critical.
Local psych support
Centralized psychological support for families was organized by Hôtel Dieu hospital in all centers receiving the injured. However, according to an article authored by the Pitié-Salpêtrière's crisis team in January, this intervention took time to implement, and was not sufficient for meeting the immediate and numerous needs of families. The task of identifying patients, escorting and informing families, as well as accompanying them to the bedsides of injured relatives on the night of 13 November was largely undertaken by the administrative team. However these staff did not feel equipped for this role and some subsequently suffered mental trauma. The article recommended that a local internal medicine team should be made immediately available for family liaison and psychological support in the event of future attacks.
This new strategy for looking after families has also been included in the hospital's revised local White Plan, according to Grenier, as has provision of psychological support for staff. This was implemented in the weeks and months after the attacks for up to 50 staff members either as one-to-one counseling or as phone and Internet sessions.



















