
DUBAI - Finding a suspicious breast lesion is just the start of the path toward optimal management and treatment of breast cancer, and multiple imaging modalities should be used, according to a talk by Dr. Rola Shaheen on the opening day of the Total Radiology sessions at Arab Health 2014.
Mammography, ultrasound, and MRI each has its role in diagnosing suspicious lesions. But establishing the radiologic-pathologic correlation is just as important to ensure concordance -- and even that's not necessarily the end of the line for radiologists looking for optimal care, said Shaheen, who is acting chair of radiology and chief of women's imaging at Mafraq Hospital in Abu Dhabi, United Arab Emirates.
Among the modalities, MRI has carved out a large and growing role in breast cancer management, but even this imaging superstar should be considered an adjunctive -- rather than primary -- modality for achieving optimal care, she said.
"It's all about optimizing breast care management and how to work as a team to save the patient," Shaheen said.
Radiologists must lead the way
Planning a diagnostic and treatment approach for breast cancer without comprehensive attention to each of the steps won't do justice to patients or their care teams, which count on the radiologist to lead the way.
 Dr. Rola Shaheen from Mafraq Hospital.
Dr. Rola Shaheen from Mafraq Hospital.
"We as the breast imagers are the major players in the multidisciplinary team in breast cancer management, or breast cancer in general, especially if the patient needs some imaging," Shaheen said. "We are consultants to clinicians to advise on what's the next best step, and we are experts on multimodality imaging and interventions including mammography, ultrasound elastography, MRI, core biopsy for fine-needle aspiration, and needle localization."
Beginning with the BI-RADS classification, it is crucial to standardize lesion classification, whether between mammographers and pathologists, technologists, or surgeons, she said.
With BI-RADS 3 lesions, for example, the finding is probably benign, but follow-up is called for and the radiologist needs to specify the short-term follow-up period. For BI-RADS 4 -- i.e., suspicious lesions -- the breast imager should subcategorize the finding into low, medium, or greater-than-medium suspicion for malignancy. By the time the breast imaging specialist gets to BI-RADS 6, a probable malignancy, the rad-path correlation should be straightforward.
Breast cancer findings include masses, calcifications, developing asymmetry, and skin thickening, which is often imperceptible, Shaheen said. For whatever reason the patient is called back -- a finding on mammography, a clinical finding, or a patient discovering a symptom -- the diagnostic path generally begins with multimodality imaging, followed by image-guided biopsy. Then comes the critical rad-path correlation and, ultimately, assessment of cancer pathology and hormonal status before deciding on treatment, which greatly depends on the individual case.
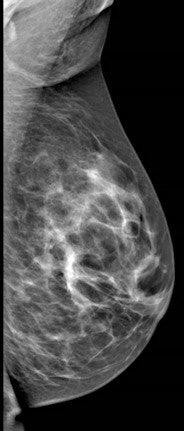
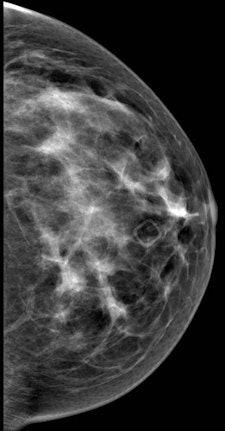 Left mediolateral oblique (left image) and left cranial-caudal (right image) unilateral diagnostic mammogram for a 42-year-old women presenting with new palpable lump in the left upper central breast with no suspicious finding on mammogram. All images courtesy of Dr. Rola Shaheen, originally appearing in the 2014 show Issue of Arab Health magazine.
Left mediolateral oblique (left image) and left cranial-caudal (right image) unilateral diagnostic mammogram for a 42-year-old women presenting with new palpable lump in the left upper central breast with no suspicious finding on mammogram. All images courtesy of Dr. Rola Shaheen, originally appearing in the 2014 show Issue of Arab Health magazine.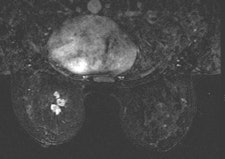
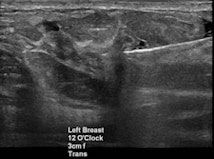 Targeted ultrasound for the palpable lump in the left breast showed vague hypoechoic area at 12 o’clock which was core biopsied under ultrasound guidance (left). Pathology of left breast ultrasound core biopsy was benign, however at multidisciplinary breast care conference, pathology result was found to be discordant with imaging findings on ultrasound, and further evaluation with breast MRI (right) showed an irregular enhancing left breast mass in the upper, central to inner breast which was confirmed to be invasive ductal carcinoma on excisional biopsy.
Targeted ultrasound for the palpable lump in the left breast showed vague hypoechoic area at 12 o’clock which was core biopsied under ultrasound guidance (left). Pathology of left breast ultrasound core biopsy was benign, however at multidisciplinary breast care conference, pathology result was found to be discordant with imaging findings on ultrasound, and further evaluation with breast MRI (right) showed an irregular enhancing left breast mass in the upper, central to inner breast which was confirmed to be invasive ductal carcinoma on excisional biopsy."Diagnosis doesn't stop with the biopsy; it's even more important to correlate the biopsy results with the imaging finding," she said.
Perhaps there are suspicious microcalcifications in a case of recurrent breast cancer. Should the patient undergo bilateral fine-needle aspiration or ultrasound-guided biopsy? Has lymph-node status been checked? Radiologists should measure not just the size of the lymph nodes but the thickness as well.
"For partially treated breast cancer that deviates from standard management, always review and/or repeat imaging and pathology exams before further management," Shaheen said.
The point is to be thorough -- and then pick up the phone to speak with the surgeon about your findings, she said.
The radiologic-pathologic correlation should be referenced by an addendum or documentation. With concordant results, give an indication of the next step. For discordant results, discuss the case with the pathologist in a multidisciplinary conference. And document the final consensus, Shaheen said.
Breast MRI
According to the 2013 American College of Radiology (ACR) guidelines, breast MRI should be performed for screening high-risk patients, as well as those with a new breast malignancy, following a 2007 report in the New England Journal of Medicine on MRI's ability to find cancer in the contralateral breast. It should also be used to screen patients with breast augmentation, which presents difficulties such as mammographically occult regions, or cancer tracking the contour of the implant, Shaheen said.
For confirmed cancers, MRI can be used to assess the extent of disease such as ductal carcinoma in situ, for additional evaluation of imaging or clinical findings, and for problem-solving.
"If you have access to breast MRI, do your patient a favor and try to get them a preoperative MRI if that does not delay their management," she said.
On the other hand, MRI is not suitable for screening the general population. It may turn up false positives or findings that are not clinically significant.
MRI may change patient management, but it is not a primary screening modality, Shaheen said.
"Breast MRI is not a substitute whatsoever for other modalities or biopsy," she said.
To conclude, preoperative multimodality imaging is essential for optimal patient management, radiologic-pathologic correlation following breast biopsy is essential to ensure concordance, and breast MRI is an important tool for a growing number of cases and may change patient management, according to Shaheen.
"Expertise, safety, and quality are important considerations for a successful breast MRI program," she said.



















