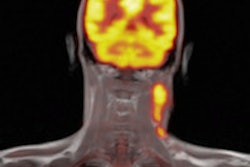
German researchers have concluded that simultaneous PET/MRI for patients with acute myocardial infarction is feasible after finding "good concordance" in a comparison of PET and MR images. The study was presented at last month's RSNA meeting in Chicago.
The results showed agreement between PET and MRI regarding myocardial viability and infarct quantification, prompting the researchers to theorize that cardiac PET/MRI could provide quantitative information on metabolic processes. That information, in turn, might be incorporated into cardiac MRI protocols to improve risk stratification in acute myocardial infarction.
The study, led by Dr. Felix Nensa from the department of diagnostic and interventional radiology and neuroradiology at Essen University Hospital, follows research published earlier this year that showed good concordance with the simultaneous acquisition of FDG-PET and MR images regarding both cine and late gadolinium-enhanced imaging.
Cardiac PET/MRI
In the current study, the researchers compared MRI and PET for both visual and quantitative assessment to determine if PET/MRI could improve imaging of acute myocardial infarction.
Nensa and colleagues evaluated 25 patients (mean age, 53 years; range, 44 to 63) who had acute occlusion of a coronary artery after interventional revascularization. PET/MRI scans were performed five to 12 days after intervention. Patients underwent an integrated whole-body PET/MRI scan, with 3-tesla field strength (Biograph mMR, Siemens Healthcare) and the PET insert inside the MRI scanner. Scan time was approximately 71 minutes (± 3 minutes).
The MRI protocol included a two-point Dixon sequence for attenuation correction, cine imaging, and late gadolinium enhancement imaging. PET scans were performed with FDG and acquisitions were electrocardiogram (ECG)-gated in one bed position with 3D image reconstruction. Visual assessment was based on coregistered short-axis slices using a 17-segment model from the American Heart Association.
Tracer accumulation in each myocardial segment was compared with regional wall motion abnormalities and with signal intensity in late gadolinium-enhanced images. The size of the infarction zone was measured on both late gadolinium-enhanced and FDG-PET images.
Image analysis
There was good agreement between PET and late gadolinium enhancement and PET and cine imaging, the researchers found. With PET, 31% of the myocardial segments showed a decrease in FDG tracer uptake, indicating an infarcted area. With late gadolinium enhancement, 28% of the infarcted myocardial segments were visible, and 24% of the segments showed abnormal wall motion with cine imaging.
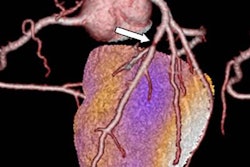
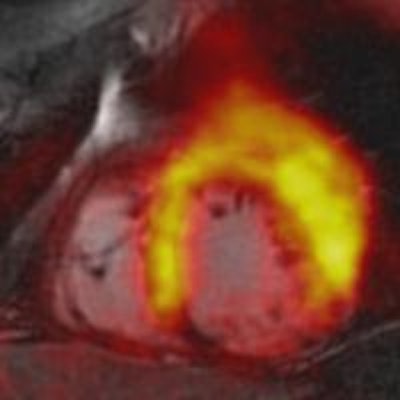
 PET/MRI of patient with acute myocardial infarction due to occlusion of the right coronary artery (RCA). The fusion shows that decreased tracer uptake (within the perfusion territory of the RCA) exceeds the area of late gadolinium enhancement. The decreased tracer uptake might delineate the area at risk. Image courtesy of Dr. Felix Nensa.
PET/MRI of patient with acute myocardial infarction due to occlusion of the right coronary artery (RCA). The fusion shows that decreased tracer uptake (within the perfusion territory of the RCA) exceeds the area of late gadolinium enhancement. The decreased tracer uptake might delineate the area at risk. Image courtesy of Dr. Felix Nensa.To better evaluate the quantitative imaging results, Nensa and colleagues developed in-house software to generate coregistered images, which compared late gadolinium-enhanced images with results from FDG-PET. Using the software in a separate group of 15 patients with visually conclusive agreement between PET and late gadolinium enhancement results, the researchers found PET defect size (35 mL) to be significantly larger than the late gadolinium-enhanced defect size (27 mL).
In addition, no late gadolinium enhancement was found in six (24%) of the 25 patients. "However, all [six patients] showed hypokinetic wall motion in the perfusion territory or in the occluded coronary artery, and all showed clearly reduced tracer uptake in that territory, which we interpreted as a stunned myocardium," Nensa said.
In conclusion, there was good overall agreement between MRI and PET in the depiction of myocardial infarction, which could potentially be included in cardiac MRI protocols to evaluate risk among patients with acute myocardial infarction, Nensa said. Further study is needed to confirm whether simultaneous FDG-PET/MRI can benefit patients with ischemic cardiac disease, he added.
Hybrid PET/MRI also could be useful with a number of different radiotracers.
"When using FDG as a tracer, I think the advantages are mainly due to the coregistration, which is inherently present in this machine," he said. "Imagine not just FDG as a tracer, but, for example, perfusion imaging with tracers with a very short half-life. You can do the perfusion imaging, while you do late gadolinium enhancement imaging, or you can compare PET perfusion imaging with MRI perfusion imaging."