FDG-PET/MRI shows similar performance to FDG-PET/CT for lymph node staging in lung cancer, with "substantial" reader agreement in determining tumor staging, according to a study published online on June 14 in European Radiology.
Using a three-segment model for attenuation correction, PET/MRI for lymph node staging in lung cancer also showed a "strong parallel" to PET/CT relative to maximum standardized uptake values (SUVmax) and diagnostic performance. Lead study author is Dr. Andres Kohan from the department of radiology at University Hospitals Case Medical Center at Case Western Reserve University in Cleveland, Ohio, U.S.
PET/MRI's promise
PET's molecular imaging capabilities and MRI's prowess with tissue discrimination through diffusion-weighted imaging is promising, according to Kohan and colleagues. "However, in the current status, the competence of MRI to provide a reliable and accurate attenuation correction map remains to be demonstrated," they noted.
While previous research has compared PET/MRI and PET/CT in a small sample of lung cancer patients, the authors added that no current literature is available dealing with interreader agreement in assessing node staging or the hybrid modalities' sensitivity, specificity, and accuracy for staging.
The study included 11 patients with suspected or confirmed lung cancer who were referred to PET/CT for staging or restaging of their disease. All patients underwent both PET/CT and PET/MRI in the same session using the same single dose of FDG. PET/CT was performed first to preserve optimal diagnostic quality of the diagnostic reference standard.
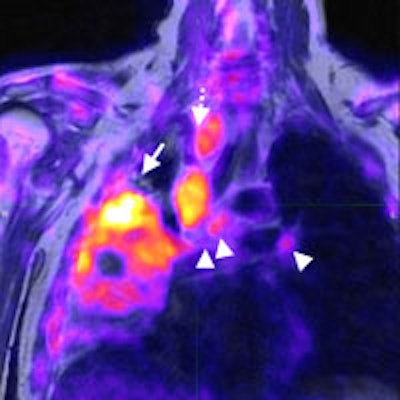
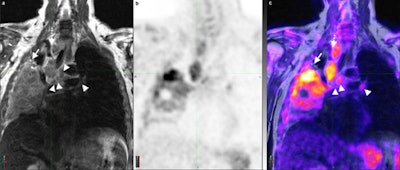 Coronal T2 turbo spin-echo sequence (a) of the chest and corresponding PET and PET/MR fusion (b, c) demonstrates a non-small cell lung cancer tumor occupying a large portion of the right lung with multiple enlarged lymph nodes (arrowheads). The superior soft-tissue contrast resolution of MRI allows for the identification of each separate lymph node and confident distinction of lymph nodes from vascular structures (dotted arrow). Similarly, atelectasis can be distinguished from tumor (arrow) even in the absence of intravenous contrast. All images courtesy of Dr. Andres Kohan.
Coronal T2 turbo spin-echo sequence (a) of the chest and corresponding PET and PET/MR fusion (b, c) demonstrates a non-small cell lung cancer tumor occupying a large portion of the right lung with multiple enlarged lymph nodes (arrowheads). The superior soft-tissue contrast resolution of MRI allows for the identification of each separate lymph node and confident distinction of lymph nodes from vascular structures (dotted arrow). Similarly, atelectasis can be distinguished from tumor (arrow) even in the absence of intravenous contrast. All images courtesy of Dr. Andres Kohan.For PET/CT, a standard dose of FDG adjusted for body weight was administered (447.7 ± 70.3 MBq) with imaging starting approximately 60 minutes after injection. PET data were acquired using time-of-flight technology on a standard PET/CT system (Gemini TF PET/CT, Philips Healthcare).
An average of nine bed positions ranging from 90 to 180 seconds each, based on a patient's weight, were acquired using PET. Low-dose CT scans of the head, neck, chest, abdomen, and pelvis also were performed for attenuation correction and anatomic localization.
The PET/MRI system (Ingenuity TF PET/MRI, Philips) included a time-of-flight PET system with a 3-tesla MRI unit next to each other in the same room. All patients underwent whole-body MRI using a 3D T1-weighted spoiled gradient-echo (GRE) sequence for tissue attenuation correction and anatomical localization.
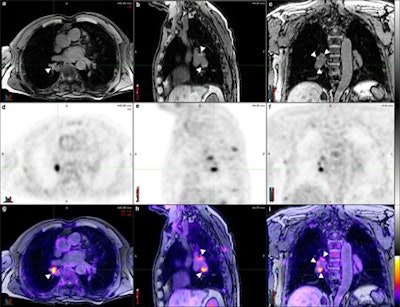 Axial (a), sagittal (b), and coronal (c) T1 fat-saturated MR images reconstructed from a volumetric 3D T1-weighted gradient-echo dataset, corresponding PET (d, e, f) and PET/MR fusion images (g, h, i). Pathologically increased tracer uptake discloses the neoplastic nature of the visualized lymph nodes. There is excellent soft-tissue contrast in MRI, which allows for the clear delineation of lymph nodes (arrowheads) and their distinction from vascular structures despite the absence of intravenous contrast.
Axial (a), sagittal (b), and coronal (c) T1 fat-saturated MR images reconstructed from a volumetric 3D T1-weighted gradient-echo dataset, corresponding PET (d, e, f) and PET/MR fusion images (g, h, i). Pathologically increased tracer uptake discloses the neoplastic nature of the visualized lymph nodes. There is excellent soft-tissue contrast in MRI, which allows for the clear delineation of lymph nodes (arrowheads) and their distinction from vascular structures despite the absence of intravenous contrast.All 11 patients completed both examinations, and no adverse events were reported. Four experienced readers reviewed the results to determine the N stage of the patients with each hybrid imaging method in a randomized blinded way.
Interobserver agreement
Overall interobserver agreement was "high" (Κ = 0.86) for PET/CT and "substantial" (Κ = 0.70) for PET/MRI among the four readers, Kohan and colleagues described. They also found full agreement among readers on the nodal stage in nine (81%) of 11 PET/CT images and seven (63%) of 11 PET/MR images.
Comparing the results between PET/CT and PET/MRI for the four readers, the researches found disagreement on the N stage for five of 44 evaluations. Four of the five cases were rated with a higher N stage with PET/MR than with PET/CT, but the difference was not statistically significant, the researchers concluded.
The diagnostic performance between the two modalities also was deemed not statistically significant. The sensitivities, specificities, positive predictive values (PPV), negative predictive values (NPV), and overall accuracies for both hybrid modalities for detecting disease (N stage > 0) and exact N stage are shown below.
| For detecting N stage greater than 0 | ||
| PET/CT | PET/MRI | |
| Sensitivity | 80% | 80% |
| Specificity | 79% | 75% |
| PPV | 77% | 74% |
| NPV | 83% | 81% |
| Accuracy | 80% | 77% |
| For detecting exact N stage | ||
| PET/CT | PET/MRI | |
| Sensitivity | 75% | 70% |
| Specificity | 79% | 75% |
| PPV | 75% | 71% |
| NPV | 79% | 75% |
| Accuracy | 77% | 73% |
PET with MRI-based attenuation correction for non-small cell lung cancer lymph node staging has a "very strong quantitative correlation to PET/CT, while it may be of a similar qualitative value," Kohan and colleagues concluded.
The results indicate that while interreader agreement is "almost perfect for PET/CT, it is still substantial in PET/MRI," they noted. "Nonetheless, we hypothesize this lower agreement was due to a learning curve in MRI interpretation, especially for nuclear medicine physicians, and the lack of other morphologic and multiparametric sequences in our PET/MRI protocol."
The potential advantage of using PET/MRI instead of PET/CT for lung cancer is not yet clear, but there may be some cases in which PET/MRI "may be superior, such as lymph node assessment," the researchers noted. "The current experience with PET/MRI in lung cancer is limited."
They recommend additional studies with morphological and multiparametric MRI sequences be conducted to better understand the role PET/MRI might play in this clinical application and to better compare the qualitative capabilities of each hybrid imaging method.