Radiation dose directives, dose management software, etc., etc. -- how can a busy radiologist keep up with it all? Medical physicist Virginia Tsapaki, PhD, shared practical and timely information about these issues at ECR 2018 in Vienna.
The Council of the European Union (EU) established directive 2013/59/Euratom, which sets basic safety standards for protection against the dangers arising from exposure to ionizing radiation. Radiologists must be aware of some key elements, including the directive's requirement that high-dose procedures such as CT or interventional radiology must be closely monitored, she noted. This applies to children in particular.
 Virginia Tsapaki, PhD.
Virginia Tsapaki, PhD."Diagnostic reference levels are mandatory and require regular review and use," said Tsapaki, from the medical physics department at Konstantopoulio General Hospital in Nea Ionia, Greece. "Clinical audits inside the radiology departments are mandatory and must be carried out in accordance with national procedures."
The directive clearly states any equipment used for interventional radiology and CT, as well as any new x-ray machine, must have a device or a feature informing the practitioner at the end of the procedure of relevant parameters for assessing the patient dose. The device or feature must also have the capacity to transfer this information to the record of the examination.
"At present, radiology centers in Europe, even if they are small practices, are required to collect and send a limited number of patient doses to their national legal authorities," Tsapaki said. "In many cases, this is done manually for each x-ray room in the hospital. This can be an extremely time-consuming and complex task."
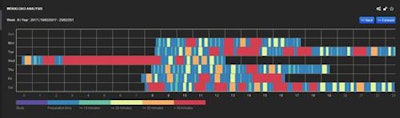
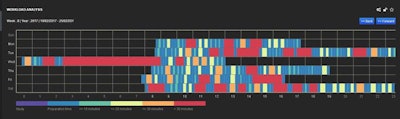
The graph shows the analysis of the weekly workload at Tsapaki's institution of the CT scanner as a function of hours and days in the week. The bar below the graph defines the colors related to the time periods of the usage. Starting from purple on the left and ending with red on the right, the color bars show the following: the actual study, the preparation time, time gap of less than 10 minutes, time gap of less than 20 minutes, time gap of less than 30 minutes, and, finally, time gap of more than 30 minutes. All images courtesy of Virginia Tsapaki, PhD.
Luckily, sophisticated software can assist in this regard, resulting in a much easier and quicker way to monitor all data included in the DICOM header of x-ray machines, or data recorded in the PACS of the hospital.
Dose management software
The users of dose management software can benchmark radiation dose levels of the hospital against national and international diagnostic reference levels. They can generate and export dose information to the examination record, explained Tsapak, who is also president of the Hellenic Association of Medical Physicists. In the case of an outlier, an alert can be generated and sent via email or a text to the medical physicist or the person in charge.
"It is very important that they are multimodality and multivendor systems and can be connected to most of the x-ray machines," she said.
A dose management system can facilitate the evaluation of general practice and workflow of the department.
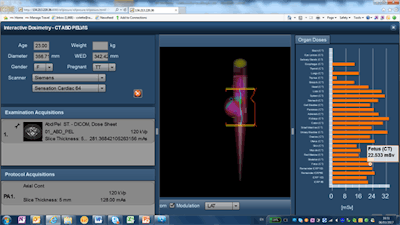
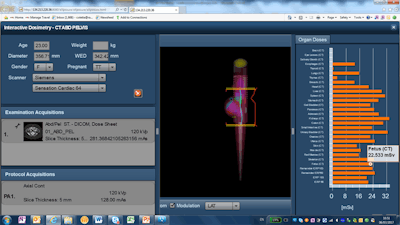
Estimation of fetal and organ radiation dose using a Monte Carlo-based calculation and a mathematical model of patient anatomy.
"It can reveal the habits of operators, so that corrective actions are made," Tsapak added. "They [systems] can help in detailed analysis of patient data for optimization of safety, quality, training, and practice of each department. The analysis of radiation dose data can be a cumbersome process that requires manual entry of thousands or even millions of values, with significant outflow of resources and the risk of typing errors."
These systems are not cheap, and the cost usually increases with the number of x-ray devices or exams performed. However, manufacturers are making strides with this software, and, consequently, costs should fall in the future. Furthermore, dose management systems do more than collect data: They are patient management tools.
"I have evaluated a number of these systems in my hospital," she said. "The software can easily provide end users with the time periods the x-ray machines are not in use. This helps a lot in order to schedule routine quality control and other routine tasks. Errors can be identified in protocol decisions that can be discussed with the radiographers, and in this way we could make corrective actions."
In the future, Tsapaki anticipates that radiation skin-dose mapping specially for interventional fluoroscopy or CT procedures will reach the market.
"This will be one additional item very helpful toward personalized patient dosimetry," she said.