The German Radiological Society's working group on musculoskeletal (MSK) imaging investigations produces guidelines for all key radiological examinations. These are designed to ensure high-quality outcomes and reliable diagnoses, as well as meet the day-to-day needs of radiologists in hospitals and independent practices.
Dr. Andrea Baur-Melnyk, head of musculoskeletal imaging at the Grosshadern Clinic in Munich, is a member of the working group's management board. In this Q&A interview, she explains the current protocol recommendations for spinal MRI measurement sequences.
Back pain is a veritable epidemic. What role does diagnostic imaging have to play in these cases?
 Dr. Andrea Baur-Melnyk from Munich.
Dr. Andrea Baur-Melnyk from Munich.Baur-Melnyk: Let's start with a few numbers. No less than 85% of Germans experience back pain at least once in their lives, and 15% to 22% suffer from chronic or recurring back pain. It's responsible for 31% of sick days and 50% of cases of early retirement on health grounds, and it costs Germany around 8 billion euros a year, so it's an extremely important social and economic issue.
Imaging shouldn't automatically be used to diagnose back pain. You don't need it for acute or nonspecific pain. Research shows that this is a costly process often associated with the chronification of pain and unnecessary intervention.
Imaging should be used for back pain only when there are red flags in the form of concomitant symptoms and previous history. These can be warning signals of a specific cause needing urgent treatment. For example, they can indicate a primary unrecognized fracture, a tumor, or an infection or, when there are radicular symptoms, a paralyzed nerve. Imaging should also be used for subacute or chronic back pain when six weeks of guideline therapy have been unsuccessful. This is based on the National Lower Back Pain Treatment Guidelines issued by associations representing the healthcare industry, physicians, and general physicians.
When should MRI be used for diagnosis?
It's useful for radicular symptoms, infections, and tumors, and that's when it's normally used. The most common cause of radicular symptoms is a herniated disk, but they can also be the result of synovial cysts and also tumors and metastases manifested in the spine and pressing on a nerve root. Nonradicular symptoms don't normally need immediate imaging.
Why has the working group issued protocol recommendations for spinal MRI sequences?
It's very often difficult to find the exact cause of back pain. Muscular imbalances and bad posture often cause it, and we can't see those in an MRI scan. Also, patients often have more than one spinal pathology, and disk herniation and facet-joint arthritis are common.
To find out exactly what's causing the pain, you need to make a precise differential diagnosis involving the patient's case history and clinical data. The protocol recommendations are intended as a guideline for colleagues in practices and in hospitals, so they use the right protocol for the right clinical matter.
What indications do they cover?
We've divided them into two main protocols. Nonenhanced spinal sequence protocols usually covers degenerative spinal changes, including degenerative disk disease, and herniation and fractures, while contrast-enhanced spinal sequence protocols should be used for tumors, metastases, and inflammatory changes. We've deliberately kept the protocols short and excluded special sequences such as diffusion, because a lot of practices can't do these.
How do you make sure these recommendations become part of clinical routine?
Whether they're actually used in practice remains to be seen, but in the radiology department at the Munich University Hospital, where I work, both protocols are displayed on all devices and always used. Our experiences have been very positive, and we want to share them with all our colleagues.
Protocol recommendations
General recommendations: The slice in all three planes should be 4-mm thick or less. The local in-plane resolution should not exceed 1 x 1 mm in the longitudinal axes (sagittal and coronal) and 0.8 x 0.8 mm axially.
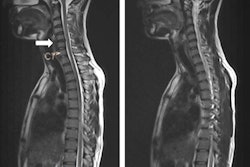
Height localization problems may occur in examinations of the thoracic spine alone. It is better to examine either the cervical and upper thoracic spine (up to about T7) or the lumbar and lower thoracic spine (from about T6).
The authors of the protocol were Dr. Rolf Janka, Erlangen University, and Dr. Andrea Baur-Melnyk, Ludwig Maximilian University of Munich.
| Nonenhanced spine MRI Indication: Degenerative spinal changes and fractures |
||
| Sequence | Planning | Remarks |
| Sagittal T1 TSE | Cervical spine: With skull base to approximately T3. Lumbar spine: From T11 to at least S3 |
Do not cut off sides in scoliosis. |
| Sagittal T2 TSE with fat saturation (e.g., STIR) | ||
| Sagittal T2 TSE | ||
| Axial T2 TSE | Strictly axial to main finding; slice thickness ≤ 3 mm if possible. | |
| Coronal T2 with fat saturation (alternatively proton density) | Incudostapedial joints and sacrum should be in FOV | T2 STIR coronal is ideal for showing sacroiliitis and sacral insufficiency fractures, transitional anomalies, and the course of the spinal nerves. |
| Optional | ||
| Sagittal T2 TSE 3D (SPACE) | From three intervertebral disk spaces, can also be measured instead of sagittal T2. | |
| Oblique sagittal T2 TSE | Approximately 45° oblique through neural foramina | Useful only for cervical spine. |
| Spinal MRI with contrast Indication: Tumors/metastases, inflammatory changes |
||
| Sequence | Planning | Remarks |
| Sagittal T1 TSE | Cervical spine: With skull base to approximately T3 Lumbar spine: From T11 to at least S3 |
Do not cut off sides in scoliosis. |
| Sagittal T2 TSE with fat saturation (e.g., STIR) | ||
| Sagittal T2 TSE | Tumour/metastases: Better to replace with T2 TSE 3D. | |
| Axial T2 TSE | With tumors, can be measured effectively with 4-mm slice. | |
| Axial T1 TSE | With tumors, can be measured effectively with 4-mm slice. | |
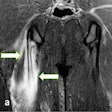
| Coronal T2 with fat saturation | Include psoas major and sacrum in FOV | Good for inflammatory changes, may not be necessary for tumor/metastasis cases. |
| IV contrast | Can also be useful for herniated disks to identify scar tissue DD relapse event after disk operation, identifying active spondyloarthritis, and identifying inflammatory processes as part of spondyloarthropathy. | |
| Sagittal T1 TSE contrast fat saturation | Measure as Dixon sequence if possible. | |
| Axial T1 TSE contrast fat saturation | Include psoas major in FOV for spondylodiskitis cases. | |
| Alternatively | ||
| Sagittal T2 TSE 3D (SPACE) | Can replace T2 sagittal. | |
Editor's note: This is an edited version of a translation of an article published in German online by the German Radiological Society (DRG, Deutsche Röntgengesellschaft). Translation by Syntacta Translation & Interpreting. To read the original version, click here.