VIENNA -- An MRI-based machine learning (ML) model showed promise in differentiating leiomyosarcoma from atypical benign leiomyoma in a study presented on 28 February at ECR 2025.
In her presentation, Dr. Kavita Shapriya, MBBS, from the Imperial College Healthcare NHS Trust in London, England reported her team’s findings, showing the high performance of their MR radiomics-based ML model, including having perfect sensitivity.
“We had pretty good results,” Shapriya told AuntMinnie.com. “The important point is that all the malignant cases were correctly identified by the model.”
 Dr. Kavita Shapriya presents her team's research on a machine-learning model based on MRI radiomics at ECR 2025. The model performed well in differentiating between leiomyosarcoma and benign leiomyoma.
Dr. Kavita Shapriya presents her team's research on a machine-learning model based on MRI radiomics at ECR 2025. The model performed well in differentiating between leiomyosarcoma and benign leiomyoma.
Leiomyosarcoma is a rare and aggressive form of uterine cancer, making up between 1% and 3% of uterine tumors. Imaging this cancer can be difficult due to features overlapping with those found on benign leiomyomas. Accurate preoperative differentiation is important for selecting the best treatment strategies.
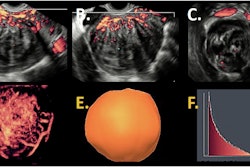
Shapriya and colleagues developed a radiomics-based ML model to improve diagnostic accuracy. The model included data collected from T2-weighted sagittal MRI sequences. These sequences were manually segmented and then optimized using a nonuniformity correction method to ensure image stability.
The researchers extracted 4,114 radiomic features, incorporating them and 11 clinical variables into several ML models. They split the data in a 70:30 ratio into training and testing sets. The team also addressed data imbalance by using an ensemble classification model with unequal classification costs. This in turn penalizes the misclassification of leiomyosarcoma.
The team tested the model’s performance on a retrospective dataset, which included 214 patients with atypical myometrial lesions who underwent surgery between 2013 and 2023. All patients had preoperative full blood count and underwent an MRI exam. Among the total cases, 193 were benign leiomyomas and 21 were leiomyosarcomas.
The final ensemble model included four clinical and six radiomic features. It performed well in the training and test sets, even though it yielded average F1 scores.
| Performance of ML model for differentiation between leiomyosarcomas, benign leiomyomas | ||
|---|---|---|
| Measure | Training set | Test set |
| Sensitivity | 100% | 100% |
| Specificity | 82% | 80% |
| Accuracy | 84% | 84% |
| Area under the curve (AUC) | 0.91 | 0.9 |
| F1 | 0.56 | 0.5 |
For the specificity measure, Shapriya said that while the model correctly identified all malignant cases, it misclassified 12 benign lesions as malignant. She suggested that the limited dataset from malignant cases may be a limitation for the current model since the disease is rare.
Still, the results support the potential for radiomics-based ML models in improving leiomyosarcoma detection, Shapriya said. She added that this offers a noninvasive and objective approach to tumor characterization.
“I certainly think it has a role to play,” she told AuntMinnie.com. “I think its role should be in enhancing how we perform at the moment and seeing how we can use that to impact our patients in a more positive manner.”
Shapriya also called for larger datasets in multicenter studies to validate the team’s results and evaluate the model’s reproducibility in real-world applications.