VIENNA -- Image-guided ablation techniques can be a suitable alternative to surgery in breast cancer patients, according to a talk given on 26 February at ECR 2025.
In his presentation, Leo Razakamanantsoa, MD, from Sorbonne Université in Paris, France, discussed the current uses of cryoablation and thermoablation, as well as their benefits toward patient outcomes and sustainability.
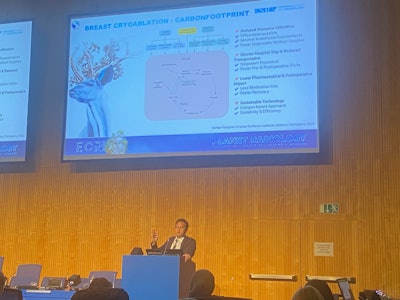 Leo Razakamanantsoa, MD, at ECR 2025 explains the advantages of ablation techniques in breast cancer treatment. He also highlighted steps that clinicians should take when considering thermoablation or cryoablation for patient care.
Leo Razakamanantsoa, MD, at ECR 2025 explains the advantages of ablation techniques in breast cancer treatment. He also highlighted steps that clinicians should take when considering thermoablation or cryoablation for patient care.
“Personalized treatment strategies are key, integrating surgical, radiotherapy, and hormonal therapy decisions based on tumor and patient characteristics,” Razakamanantsoa said.
Ablation techniques have become more popular in recent years as a quicker, less painful, and less time-consuming method for treating a variety of cancers. Previous studies suggest that they are successful in breast cancers of various sizes, including large tumors.
One study published in 2024 highlighted results of the ICE3 Trial, which showed that cryoablation plus endocrine therapy led to 96.3% of breast cancer patients being free of local recurrence. It also reported no significant adverse events and no scarring or changes to the shape and size of treated breasts.
The two versions of ablation include thermoablation, where cancers are “cooked” with heat either through radiofrequency or microwave energy, and cryoablation, where cancers are killed via extreme cold. Ultrasound is the go-to imaging modality for guiding ablation.
Razakamanantsoa said that several steps need to be taken before either ablation technique is used on patients. These include the following:
- Comprehensive patient review: This includes gathering relevant information such as a patient’s medical history, comorbidities, prior surgeries, imaging and biopsy results, tumor characterization, and intervention indications.
- Multidisciplinary approach: Here, tumor board discussion is needed for treatment validation. Anesthesiologists should also be consulted for sedation assessment.
- Patient consolation: Patients need to be explained the procedure, including its goals, expected outcomes, and possible side effects and complications. Clinicians meanwhile need to obtain informed consent, both written and oral.
- Technical planning: This includes considerations for image guidance and positioning, equipment and materials preparation, scheduling, and hospital admission logistics.
- Preoperative requirements: Operating clinicians should assess for coagulation, order a preoperative MRI for final evaluation, and prepare the patient. For the latter, this includes hygiene, fasting, and IV access.
Razakamanantsoa said that ablation has several advantages in breast cancer treatment, such as minimal invasiveness, a reduction in hospital stays, an improvement in aesthetic outcomes, and a lower carbon footprint.
For environmental sustainability, he outlined ablation’s minimal anesthesia requirements, fewer disposable medical supplies used, cryogen-based approach, and lower medication dose used, among others.
“In general, we need personalized treatment strategies and refine the technological advancements to continue to be part of the course of treatment,” Razakamanantsoa said.
For more coverage from ECR 2025, visit our RADcast on AuntMinnieEurope.