Anything can happen three years from now, but that's not stopping breast imaging experts from making predictions for modalities within the next few years at ECR 2022 in Vienna.
Presenters on 13 July made predictions for what to expect in the year 2025 for breast MRI and ultrasound, as well as how advances in the clinical setting can lead to more saved lives from breast cancer through early and more accurate detection.
"No one has a crystal ball, so that's exactly why we organized this session," said session moderator Dr. Hilde Bosmans from the University Hospital of Leuven.
Researchers have been working to find out ways to improve breast screening protocols while also easing patient burden. With so many techniques, combinations of modalities, and advances in technology, it can be challenging for radiologists to adjust to the new information that comes with them.
Bosmans said there are several aims for new breast imaging in the future. These include reducing patient discomfort, increasing small lesion detectability, improving radiological cancer workup and treatment, reducing mortality, and improving quality in society.
"[This] starts with improving current technology for all women and for specific subgroups worldwide," said Bosmans, who was the session's moderator.
Breast MRI in 2025
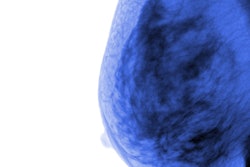
Supplemental breast MRI has been touted over the years for its superior sensitivity to conventional mammography but falls short in specificity. This issue could lead to unnecessary follow-up work, such as biopsy. Along with that, recent research suggests that contrast-enhanced mammography could be a suitable alternative to MRI with comparable accuracy and better accessibility.
In his talk, Dr. Pascal Baltzer from the Medical University of Vienna talked about MRI's advantages, such as higher sensitivity and negative predictive value, as well as comparable specificity.
"I think there will always be a role for breast MRI," he said. "That doesn't mean that contrast-enhanced mammography doesn't have an attractive method, but I don't think it will replace breast MRI."
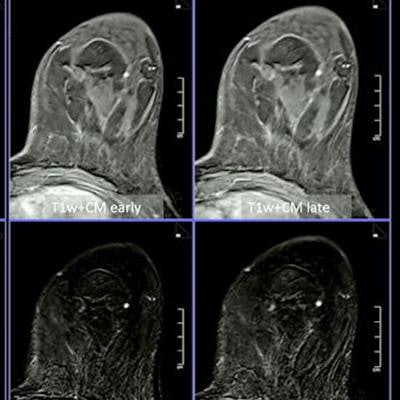
 Dr. Pascal Baltzer from the Medical University of Vienna talked about breast MRI's outlook for 2025. He said shorter protocols incorporating diffusion-weighted imaging and machine learning can help improve image quality and detection of malignancies. Images courtesy of the ECR.
Dr. Pascal Baltzer from the Medical University of Vienna talked about breast MRI's outlook for 2025. He said shorter protocols incorporating diffusion-weighted imaging and machine learning can help improve image quality and detection of malignancies. Images courtesy of the ECR.Baltzer said that he expects MRI protocols to be shorter in 2025, with a magnet time of less than 10 minutes. This, he said, can be accomplished with diffusion-weighted imaging (DWI) and T1-weighted dynamics. Acceleration techniques using artificial intelligence (AI) could also help in reconstructing images and abbreviated protocols, he added.
"In 2025, I would predict good quality MRI imaging and reporting that improves the acceptance of MRI itself," he noted. "I also hope that this will be part of European Society of Breast Imaging (EUSOBI) recommendations (i.e., updated indications for breast MRI regarding problem-solving and screening)."
Other improvements Baltzer predicts will be implemented in 2025 include the usage of common lexicon, applying the Kaiser score when using machine learning for imaging, greater usage of DWI to help prevent unnecessary biopsies, more evidence in screening women with dense breasts and treatment response, and ending the usage of abbreviated first-pass imaging.
Breast ultrasound in 2025
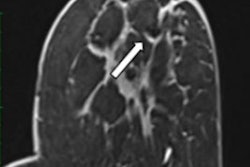
The future of ultrasound in breast imaging is bright, with ultrafast imaging on the horizon, said Dr. Chris de Korte from Radboud University Medical Center in the Netherlands.
"In ultrasound imaging, there's really a revolution going on," he said.
Ultrafast imaging is a relatively new concept in ultrasound imaging. Previous research suggests that ultrafast imaging can capture images at frame rates up to 100 times faster than conventional imaging. This includes improved penetration and lateral resolution, as well as similar contrast.
Among the predictions de Korte made for ultrasound in the breast imaging setting to coincide with ultrafast imaging were improvements in image quality, real-time 3D imaging, and contrast-enhanced ultrasound (CEUS).
 Ultrafast ultrasound imaging will play a more prominent role in supplemental breast cancer screening in 2025, said Dr. Chris de Korte from Radboud University Medical Center in the Netherlands. The ultrasound "revolution" de Korte said is happening will eventually result in combining 3D, functional, and contrast-enhanced techniques.
Ultrafast ultrasound imaging will play a more prominent role in supplemental breast cancer screening in 2025, said Dr. Chris de Korte from Radboud University Medical Center in the Netherlands. The ultrasound "revolution" de Korte said is happening will eventually result in combining 3D, functional, and contrast-enhanced techniques.However, de Korte didn't stop his predictions in 2025. In 2027, 3D functional imaging and super-resolution imaging will be present, he said. And in 2030, the final goal of combining 3D, functional, and contrast imaging will be realized.
"All this technology might not be decisive, but if you combine them to have the whole package and use a lot of information, then the detection and characterization may be much better," he added.
Breast imaging clinics in 2025
Radiologists have a major role in the interdisciplinary setting and will have an increased role in treatment guidance and monitoring, said Dr. Eva Maria Fallenberg from the Institute for Diagnostic and Interventional Radiology in München in her talk.
Fallenberg also said radiologists will have an increased role in providing risk-adapted pathways and that they will be accompanied by AI tools to help reduce screening workload, reduce symptomatic routine screening, and define individual risk situations.
With improving imaging technology comes earlier detection of cancer. While this helps with mortality rates, it also means more cancer cases. Fallenberg said that compared with 2020, new cancer cases will increase by 9.73% in 2040 due to demographic changes.
Breast imaging is influenced by several factors today, including mammography screening, radiologist shortages, environment, and breast density, among others. Variation in population can also influence breast imaging since research has shown that breast cancer affects subgroups differently and that individual risk should be prioritized.
"In the images, there is a lot about the risk of the patient," Fallenberg said. "So, we have the chance to identify the risk."
Fallenberg added that with increasing roles in the treatment pathway, radiologists need to be aware of side effects from treatments and staging and that they should be part of the core multidisciplinary team when it comes to planning.
"From our perspective, the important impact of the radiologist is underrepresented in this composition. We have to be in the core system somehow," she said.