Diffusion-weighted MR imaging models can differentiate between malignant and benign breast lesions, according to research presented on 11 May at the International Society for Magnetic Resonance in Medicine (ISMRM) meeting.
In his presentation, Dr. Wang Hongjie from Jining Medical University in China found high interobserver agreement and diagnostic efficiency in models combining diffusion-weighted imaging (DWI), intravoxel-incoherent-motion diffusion-weighted imaging (IVIM), and diffusion kurtosis imaging (DKI).
"[The combined models] have demonstrated to be a robust tool in differential diagnosis of benign and malignant TIC type II lesions," Hongjie said.
The ISMRM is holding this week's meeting in conjunction with the European Society for Magnetic Resonance in Medicine and Biology and the International Society for MR Radiographers and Technologists.
Preoperative diagnosis can be challenging
More than half of breast cancer diagnoses show a type-III time-intensity curve (TIC) on dynamic contrast-enhanced MRI. However, about 34% of breast cancer cases show a type-II curve, and about 11.5% of benign breast lesions also present with type-II curvature.
Hongjie said this overlap between benign and malignant TICs on type-II breast lesions makes preoperative diagnosis challenging.
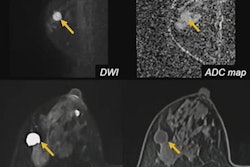
While dynamic contrast-enhanced MRI has high sensitivity, it also has low specificity for breast lesions with a type II TIC. DWI has been looked at in recent years in classifying breast lesions without the use of a contrast agent. DWI measures water motion in tissue, including malignant lesions, by using diffusion-sensitizing gradients while acquiring images. Breast malignancies show restricted diffusion compared to normal breast tissue, and they present as bright spots.
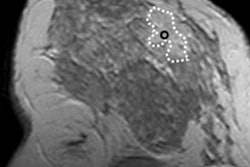
 Diffusion-weighted MR imaging models can differentiate between malignant and benign breast lesions, according to research presented at the ISMRM annual meeting. Here, a 56-year-old woman presents on DWI with a mass in the outer-inner quadrant of the left breast. The pathological diagnosis of this mass was phyllodes fibroadenoma. Image courtesy of Dr. Wang Hongjie.
Diffusion-weighted MR imaging models can differentiate between malignant and benign breast lesions, according to research presented at the ISMRM annual meeting. Here, a 56-year-old woman presents on DWI with a mass in the outer-inner quadrant of the left breast. The pathological diagnosis of this mass was phyllodes fibroadenoma. Image courtesy of Dr. Wang Hongjie.While DWI with apparent diffusion coefficient (ADC) is used to diagnose different types of breast lesions, IVIM allows for assessment of tissue diffusion and perfusion information simultaneously. DKI, meanwhile, evaluates the diffusion of water molecules in breast tumors, which can't be performed with either of the aforementioned techniques.
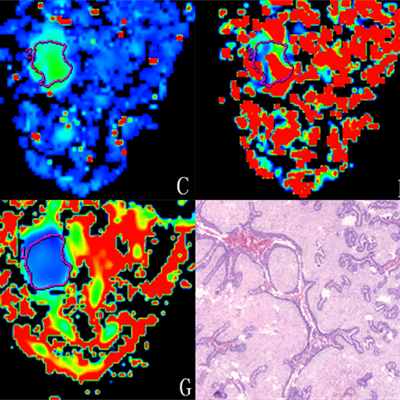
These three diffusion models have not been combined to differentiate malignant from benign type-II TIC breast lesions so far, which is what Hongjie et al wanted to do. The goal was to see if combining the models could improve the diagnostic accuracy of different types of TIC type-II breast lesions.
The team retrospectively looked at data from 103 women with an average age of 49 years. The women underwent all three preoperative diffusion methods and had TIC type-II breast lesions confirmed by pathology. They were divided into a benign group (25 lesions in 25 patients) and a malignant group (78 lesions in 78 patients).
Two senior observers manually described regions of interest at the largest solid part of tumors independently.
The researchers found that the three diffusion models achieved the greatest diagnostic efficiency when combined, with an area under the curve of 0.915, sensitivity of 92.3%, and specificity of 84%.
Diffusion characteristics of malignant lesions included lower ADC, true diffusion coefficient, and mean diffusion rate, as well as higher perfusion fraction and mean kurtosis values than that of benign breast lesions.
"The IVIM parameter of the true diffusion coefficient and the DKI parameter of mean kurtosis were shown as independent influencing factors," Hongjie and colleagues wrote.
The study authors also found "excellent" interobserver agreement of each diffusion parameter measurement, with intraclass correlation coefficients being above 0.75.
They concluded that this combined approach differentiates lesions better than DWI alone and could help in accurate preoperative prediction of benign and malignant breast lesions, which they called "essential" in clinical practice.