Advances in data mining from radiological cases can be made only if the global imaging community adopts lexicon and formatting standards for their reports, and radiologists must ask their IT providers for reporting tools, especially support for the International the Healthcare Enterprise Management of Radiology Report Templates (IHE MRRT). Only then can structured reporting have a substantial impact on clinical decisions and workflow in a way that will revolutionize both daily practice and data extraction, according to speakers at this afternoon's session.
The current lack of report standardization across all disciplines forms one of the key challenges to workflow and patient management due to inconsistency between different institutions, departments, and among individual radiologists. A joint initiative between the European Society of Radiology (ESR) and the Radiological Society of North America (RSNA), RadReport (www.radreport.org), introduced two years ago and formalized last year in a memorandum of understanding, aims to promote and facilitate structured reportingthrough the creation of a joint open repository for radiology report templates.
The initiative, to be announced to ESR members during ECR 2015, uses the RSNA's web infrastructure. Contributions will be free from copyright. Furthermore, authors and centers will be referenced but will not be liable for how their templates are used.
Experts believe the joint efforts of the two societies will be more effective than each society working separately on their own repositories. The adoption of structured reporting through the use of standards such as MRRT and the incorporation of lexicons such as Radlex will allow large-scale data extraction and make content truly universal, according to Dr. Osman Ratib.
Experts believe the joint efforts of the two societies will be globally more effective than each society working separately on their own repositories.
"I am hoping that the session will show radiologists how to improve their reporting structure -- and demonstrate that the added value it will bring to our medical future is worth the effort," said Dr. Osman Ratib, chair of ESR's eHealth and Informatics subcommittee, and also professor at the University of Geneva and head of the Nuclear Medicine and Molecular Imaging Division. "We can either impose standardization through top-down decisions, or achieve it by consensus. We believe it is preferable to take a bottom-up approach."
ESR members, who have already worked on standardization in their different fields, and even internally in their respective institutions, will be able to share their data. Doctors will eventually be able to select the most applicable reporting models. Reporting methods that work will be adopted, while those that don't will be discarded. In this way, the repository will be based on natural selection and function similarly to social networks.
In an age of evidence-based medicine, it is hoped that the adoption of structured reporting through the use of standards such as MRRT and the incorporation of lexicons such as Radlex will allow large-scale data extraction, made possible with tag tools that will attach the Radlex lexicon to sentences or items in the report. An invisible code tagged to certain words will mean that different terminology such as "liver mass," "metastases of the liver," "liver metastases" or "cancer of the liver" will no longer stop doctors finding the information they need.
 The joint ESR/RSNA team, which includes the Template Library Advisory Panel, met for the first time at a "kick-off" meeting at RSNA in December 2014. Dr. Osman Ratib is second from left.
The joint ESR/RSNA team, which includes the Template Library Advisory Panel, met for the first time at a "kick-off" meeting at RSNA in December 2014. Dr. Osman Ratib is second from left."It is important to use tags as this will make the report's essential content globally accessible for nonspeakers of the original language," Ratib noted. "Radiologists must fully understand why they should make the effort to standardize reports in MRRT format and with the Radlex code: only then can reports become truly universal, regardless of the original language they were written in."
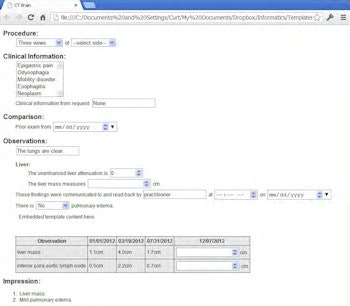
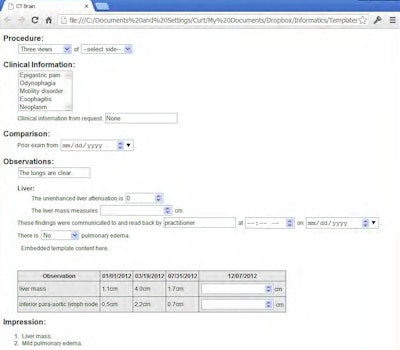
Delegates will also learn how structured reporting can allow them to take full advantage of the potential of quantification, categorization, and scores.
"Clear categorization, scoring, and coding is not often used in general radiology and in radiology in general. Such elements could be more easily used in structured reporting and this would make it easier to link findings and images," stated Dr. Peter Mildenberger, vice chair of the radiology department and responsible for radiology IT at the University Medical Center in Mainz, Germany.
Words might be too unclear for description or recommendation, and cannot adequately pinpoint whether the image shows a tumor, inflammation, or nothing. Descriptions may differ depending on language, and even within the same language, terminology may vary. Furthermore, radiologists may use the same expressions for differing degrees of certainty.
 Structured reporting has potential for workflow improvement, specifically through codes that generate automatic prompts which act as decision support, according to Dr. Peter Mildenberger.
Structured reporting has potential for workflow improvement, specifically through codes that generate automatic prompts which act as decision support, according to Dr. Peter Mildenberger."Describing a pathology with the phrase 'it could be,' is not helpful. By this, one radiologist might mean that he or she strongly believes it is the pathology in question, another that it is simply a possibility. Therefore, prose may generate huge discrepancies in interpretation," said Mildenberger, who is also a cardiovascular, emergency, and oncology imaging consultant.
Moreover, it is difficult and time-consuming for physicians to access the relevant information that might be hidden within the long radiology report that sometimes has no conclusion and up to 10 differential diagnoses, he continued.
"My secondary message is structured reporting's large potential for workflow improvement, specifically through codes that generate automatic prompts. This can't be done easily with prose reports," he noted.
Mildenberger points to systems that already incorporate structured reporting in decision support, citing one Boston group as a case in point. Its system provides automatic recommendations based on a category of findings and accepted guidelines. For example, a 6 mm lung nodule in a low-risk patient will automatically generate a recommendation to recall the patient in six months.
Attendees will also learn how to write reports in the MMRT HTML 5 format, as well as upload templates to the server. The repository already contains a large sample of templates, and groups from other countries have started to adopt these, and also contribute their own.
In addition, there will be a chance to question the value of the reporting initiative during the panel discussion, as well as discuss how to measure the value of structured reporting.
"So far there is no concrete evidence that proves its strongly suspected benefits -- is this a new area for a multicenter study?" Mildenberger said.
The future for structured reporting and its role in the radiological workflow is not yet clear cut. Turkey's Ministry of Health, for instance, wants its radiology departments to adopt structured reporting. There is, however, a chance that change will not come quickly enough if the IT companies don´t follow suit. Reporting tools for BI-RADS or PI-RADS affect a small part of total imaging, while there are still many other imaging procedures for which IT systems don't yet provide templates, he explained.
"If radiologist groups implement structured reporting and surgeons and physicians start requesting it, then there will be pressure on all radiologists to adopt it, and they in turn will put pressure on vendors to incorporate structured reporting tools in their software, rather than obliging imagers to rely on the authoring tools provided by the ESR and RSNA joint initiative," he added.
Ratib echoed these comments.
"Radiologists must therefore request manufacturers to adapt their software so that every template can be easily incorporated into RIS and PACS. There should also be tools to allow users to easily make reports in the required formats, create new templates, and upload them to the repository," he remarked.
Originally published in ECR Today on 4 March 2015.
Copyright © 2015 European Society of Radiology