Independent teleradiology in the U.K. is in a growth phase as radiology service provision in the National Health Service (NHS) is under pressure and new models of healthcare emerge.
Radiology has been a victim of its success. It has expanded and become more sophisticated, and clinical radiologists have moved into a much more central position in patient management for both emergency and planned care.
 Dr. Stephen Davies.
Dr. Stephen Davies.
Radiology service provision is becoming more diverse in the U.K. and the standard NHS radiology model of service delivery is changing. So where does teleradiology fit into this? Well, one view is that it complements and partners NHS provision.
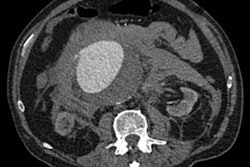
Let's have a look in a bit more detail. The original teleradiology services were introduced to supplement hard-pressed on-call night services where rotas were short of radiologists. Increasing demand at night from changing practice -- National Institute of Health and Care Excellence (NICE) stroke and NICE head injury guidelines together with changing emergency care practice in medicine and surgery -- have led to a rapid growth in night work. Experienced regular nighthawk radiologists may rightfully become experts in emergency radiology.
The emergence of PACS has been a key facilitator in the growth of teleradiology. The ease of image transfer has provided the opportunity to export large volumes of imaging data. Now the major component of teleradiology workload is the daytime routine and emergency reporting.
This provides the opportunity for traditional radiology departments to have a scalable quality-assured extension to their service. Planned and unplanned gaps in radiology reporting capacity may be delivered, and departmental reporting standards can be maintained by teleradiologists who have in depth experience practicing in the NHS.
Quality
Understandably, the bar is set high in the U.K. independent sector. The teleradiology quality framework includes service delivery and clinical elements. Clinical quality processes could be regarded as an exemplar to the NHS.
Discrepancy recording, review, and arbitration, together with radiologist reflection and learning, all contribute to a robust process. Rightly, U.K. radiology should be proud of the standards it aspires to and delivers. Teleradiology has its part to play in meeting those standards.
Audit is a key activity, and typically 10% of cross-sectional imaging is audited. This is certainly greater than the standard NHS department, and represents a key investment for teleradiology companies and good learning opportunities for the radiologists.
Concerns
Two concerns emerged at a recent debate at the U.K. Radiological Congress (UKRC) 2013: Teleradiology does not support teaching and teleradiology reports are not always sufficiently focused for multidisciplinary team (MDT) meeting use.
Taking the first point; the current model does not provide teaching opportunities for trainees, but what it can do is to provide the opportunity to outsource reporting and create time for "in-house" teaching.
On the MDT point there is a definite trend toward subspecialization in teleradiology as has happened in radiology departments across the U.K. This will result in increasingly focused and relevant reports to support MDTs.
Face-to-face is key to modern radiology -- formal clinical consultations in MDTs and out of MDTs; case management discussion and intervention. These are good reasons for in-house nonteleradiologists. However, teleradiology has an increasingly established place in complementing these activities and in supporting the service.
Future
Looking into the future, U.K. teleradiology will probably become an accepted part of the service delivery model for hospitals where they run a hybrid in-house and outsourced service. The latter is scalable and quality-assured and can be tailored to the department needs.
We will see a variety of service providers in the U.K. as the Any Qualified Provider (AQP) model becomes established in the English NHS. Although this runs the risk of fragmentation of services and potential destabilization of NHS departments, there are opportunities for innovation in service delivery. PACS will enable image transfer, and the trend toward vendor-neutral archiving will help a more diverse imaging market.
With the development of a greater level of seven-day working, innovation will be required, and teleradiology will for some NHS departments assist in meeting this aspiration.
Nighthawk teleradiologists will -- by virtue of volume and robust feedback and the learning opportunities that audits provide -- become recognized experts in emergency imaging. Teleradiology companies need to use this resource in a broader educational context and provide teaching for trainees and established consultants.
Radiologists will develop portfolio careers with contracts in the NHS, and independent sector and the traditional "private practice" model could decline as insurance providers apply increasing pressure and a greater diversity develops in the independent sector.
The knowledge accrued in the sophisticated quality and service delivery models can be of benefit to the delivery of radiology to our patients.
In summary, teleradiology in the U.K. is growing and has moved from a low-volume nighthawk service to providing significant volumes of radiology reporting and working in partnership with the NHS to complement existing service provision. Emerging models of radiology services will be supported by teleradiology as a scalable quality assured option.
Dr. Stephen Davies is a radiologist in Cwm Taf Health Board, a former president of the British Institute of Radiology (BIR) (2010-2012), and recently became medical director of Medica Reporting, the U.K.-based teleradiology company.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.