The start of organized CT lung cancer screening in the U.S. in 2013 has helped avert more than 10,000 deaths from the disease between 2014 and 2018 due to earlier cancer detection, according to a study published on 30 March in the BMJ.
But did all patients benefit from this positive effect? Perhaps not, wrote a team led by Alexandra Potter of Massachusetts General Hospital in Boston. Although in general the results are good news for people at risk of lung cancer, Black, Indigenous, and people of color (BIPOC), as well as those living in less educated and lower-income areas, may not be benefiting as greatly.
"We found disparities in the stage of lung cancer at diagnosis among subgroups of patients," Potter and colleagues reported. "Patients who were non-Hispanic white and patients living in better educated and higher-income areas were more likely to have stage I disease than stage IV disease at diagnosis."
Early detection is key
Although treatments for late-stage lung cancer have improved, early detection and treatment remain the best way to curb mortality rates from the disease, Potter's group noted. Yet despite evidence from the U.S. National Lung Screening Trial (NLST) that shows lung cancer screening with low-dose CT is effective at reducing death rates, skeptics remain.
So Potter's team sought to assess the effect of low-dose CT lung cancer screening on cancer stage shift, survival, and any patient-related healthcare disparities related to disease stage, based on the U.S. Preventive Services Task Force's (USPSTF) 2013 guidance (i.e., annual low-dose CT screening for lung cancer for adults between the ages of 55 and 80 with a 30 pack-year smoking history. This recommendation changed in 2021, when the task force expanded it to include people between the ages of 50 and 80 with a 20 pack-year smoking history).
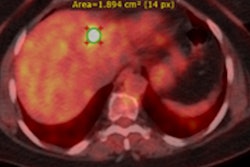
The authors conducted a study that included data from the Surveillance Epidemiology End Results (SEER) program database regarding 763,474 patients between the ages of 45 and 80 diagnosed with non-small cell lung cancer (NSCLC) between January 2010 and December 2018. They estimated annual percent change in percentage of stage I lung diseases among those 45 to 54 years of age (eligible for screening) and those 55 to 80 years of age (potentially eligible), adjusted odds ratios for year-to-year changes in likelihood of having earlier stages of disease at diagnosis, and adjusted hazard ratios for changes in hazard of death before and after screening was introduced.
Potter and colleagues found that the 2013 guidelines appeared to improve lung cancer metrics such as stage at diagnosis and all-cause survival.
| Effect of 2013 CT lung cancer screening guidance on cancer metrics | ||
| Measure | 2010- 2013 | 2014-2018 |
| Percentage of stage I NSCLC (patients ages 55 to 80) | 27.8%-29.4% | 30.2%-35.5% |
| Odds of patients having one lung cancer stage lower at diagnosis | 2.3% | 8.7% |
| Median all-cause survival of patients 55 to 80 | 15.8-18.1 months | 19.7-28.2 months |
These improvements were positive. But they didn't necessarily translate to BIPOC individuals, who tend to be at higher risk compared to their white counterparts for later-stage lung cancer.
In fact, the researchers found that although in 2010 stage IV disease was the most common among people of all races and ethnicities between the ages of 55 and 80, by 2018, more white patients in this age group had stage I disease than stage IV disease -- a result that corresponded to the income and education of these individuals. Yet BIPOC patients and those living in lower-income or less-educated regions continued to be more likely to present with stage IV lung cancer in 2018, Potter and colleagues noted.
"Our findings ... highlight disparities between certain patient populations in the stage of NSCLC identified," they wrote. "Previous studies have shown that the USPSTF lung cancer screening guidelines preclude screening of many women and racial minorities at high risk, given their lower pack-year smoking history and earlier age at diagnosis of lung cancer compared with white men diagnosed as having lung cancer."
Focused effort
Mitigating healthcare inequities takes focused effort, according to Dr. Anna Melzer of the University of Minnesota and Dr. Matthew Triplette of the Fred Hutchinson Cancer Research Center in Seattle. The two wrote an editorial that accompanied the work of Potter's team.
"Equitable access to screening that reduces health disparities requires targeted multilevel intervention," Melzer and Triplette noted. "Researchers and policymakers must analyze not just how many people are being screening but also the 'mismatch' between who is screened and who bears the greatest burden of disease related to lung cancer."