The German Cardiology Society (DGK) and the German Radiological Society (DRG) have published a joint consensus paper on carrying out MRI examinations on patients with pacemakers and implantable cardioverter defibrillators (ICDs). In this interview, lead author Dr. Torsten Sommer, head of the Diagnostic and Interventional Radiology Department at the German Red Cross Hospital in Neuwied, Germany, explains the aim of this initiative and why it can improve MRI access for this patient group.
DRG: What is the clinical relevance and importance of the consensus paper?
 Dr. Torsten Sommer from Neuwied in Germany.
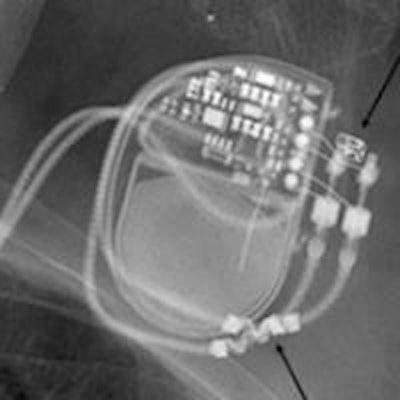
Dr. Torsten Sommer from Neuwied in Germany.Sommer: In Germany alone, there are around one million patients with active cardiac implants, e.g., pacemakers and ICDs. This number is increasing, particularly in terms of ICDs, mainly because of demographic changes. If such a large group of patients doesn't have access to MRI, which is often the best imaging technology for diagnostics and therapy planning, this causes major problems for patient care.
The good news is that intensive international research, including work by German radiological bodies, has significantly improved the situation for pacemaker and ICD patients over recent years: people with conventional pacemakers or ICDs can now be examined using "off-label" procedures, subject to certain safety precautions. And we now have MRI-safe pacemakers and ICDs that are certified and authorized for use under specific conditions.
That sounds like a positive development. But what's the catch?
The problem is that it is still very difficult for most pacemaker and ICD patients to get an MRI scan -- even for those fitted with the new devices that are conditionally MRI-safe. This is partly because referrers, cardiologists, and radiologists don't know enough about this new and complex subject, and also because no clear procedures and responsibilities have been defined for radiologists and cardiologists working together.
We do have publications by individual associations: the 2013 European Society for Cardiology (ESC) guidelines and the DRG's 2015 position paper. Where does the DGK and DRG consensus paper fit in?
I have great respect for cardiology guidelines. However, the relevant chapter of the ESC publication deals with the whole subject in just two pages of highly simplified recommendations that don't reflect the complexity of the issue. For example, it leaves out key safety aspects such as pulse oximetry monitoring of patients, and nearly all the controllable risk management aspects of MRI technology. These include the ability to reduce high-frequency energy input by modifying MRI sequence parameters.
And what was the purpose of the DRG's 2015 paper?
The DRG's 2015 position paper was a response to the ESC publication and provided a detailed description of the radiology and physics of MRI in pacemaker patients. It reinforced, expanded, and in some cases, corrected, the ESC paper.
The new DGK and DRG consensus paper is the logical next step after these publications, setting out the two associations' objectives and ratified by both bodies. It clearly defines the interfaces between radiology and cardiology, provides harmonized and jointly ratified risk assessment and patient monitoring procedures, and presents specific reprogramming options for pacemaker and ICD systems that have been optimized for patient safety and clinical practicability.
What was it like working with your cardiology colleagues?
There were some tensions and political turf wars at first, and we exchanged a few strongly worded emails. But later on, as we discussed the issues involved and shared our specialist expertise in cardiology, electrophysiology, MRI physics, and radiology, we developed a very good, fruitful, and professional relationship.
As the authors, we're delighted the consensus paper has been brought to a successful conclusion. It's taken two years of work and five approval bodies, but there has been no significant friction or editing cuts!
The consensus paper is a major step forward for both disciplines. How important is it, and what are its objectives?
It is the world's first published consensus document between national radiology and cardiology bodies to make specific joint recommendations on the procedural management of MRI exams in pacemaker and ICD patients. Its purpose is obviously to maximize patient safety, and to create a legally and clinically workable procedure for broader and better MRI care, even for patients who aren't treated in specialist institutions.
Can we expect any new technological developments in this field?
Definitely. Manufacturers are developing pacemaker and ICD systems with automatic magnetic field detection, which would significantly increase practicability due to the possibility of primarily local- and time-delayed reprogramming of the systems. And although MRI manufacturers have been very reticent about the issue for the past 10 years, they're now making an important contribution through new software development and user interfaces that allow better control of safety parameters when examining patients with active and passive implants.
Editor's note: This is an edited version of a translation of an article published in German online by the German Radiological Society (DRG, Deutsche Röntgengesellschaft). Translation by Syntacta Translation & Interpreting. To read the original article, click here.