Using a combination of several modalities, including PET/CT, to achieve an accurate diagnosis is vital to reduce the likelihood of surgical failure and the risk of complications in cases of persistent or recurrent primary hyperparathyroidism (PHPT), researchers from a leading London facility have reported.
Hyperparathyroidism occurs when the parathyroid glands create too much parathyroid hormone (PTH) in the bloodstream. PHPT is characterized by hypercalcemia and is a surgically treatable cause of morbidity. Preoperative localization is essential prior to a minimally invasive parathyroidectomy, which carries fewer risks than four-gland exploration, according to Mitesh Naik, honorary clinical research fellow, and colleagues in the Department of Imaging, Imperial College Healthcare NHS Trust.
"First-line modalities include ultrasound and parathyroid scintigraphy (sestamibi), which are frequently used in combination. Second- and third-line modalities include 4D CT, MRI, PET/CT [F-18 fluorocholine and C-11 methionine], and angiography and venous sampling, with availability and use dependent on local expertise," they stated in a digital poster at RSNA 2020 that received a certificate of merit. "You must identify parathyroid adenomas using conventional and novel modalities."
Parathyroidectomy is the only cure for PHPT. Traditionally, this involves open surgery and four-gland exploration, for which imaging is not essential. Over the past decade, image-guided minimally invasive approaches have been used, and the benefits include cosmesis, fewer complications, and reduced length of hospital stay.
| How to manage surgery for primary hyperparathyroidism cases | |
| Measure | Criteria for surgery |
| Age | < 50 |
| Serum calcium | ≥ 1 mg/dl above upper limit of normal |
| 24-hour urinary calcium | > 400 mg/day |
| Estimated glomerular filtration rate | < 60 ml/min |
| Biochemical stone profile | Increased risk |
| Renal imaging | Nephrolithiasis or nephrocalcinosis |
| Vertebral imaging | Vertebral fracture |
| Bone mineral density | T-score ≤ 2.5 |
Parathyroidectomy is recommended for all symptomatic patients and for asymptomatic patients if there is evidence of subclinical (musculoskeletal or renal) end-organ effects or risk of disease progression, they explained.
The incidence is around 0.4 to 82 cases per 100,000. Sporadic PHPT (90%-95% of cases) increases with age, and it is more common in women than men and in the African American racial group. Inherited/familial PHPT (5%-10% of cases) is associated with certain syndromes, including multiple endocrine neoplasia types 1, 2A, and 4.
Patients with classical PHPT present with the following:
- Musculoskeletal: osteitis fibrosa cystica, reduced bone mineral density, bone pain, fractures, muscle weakness
- Renal: nephrolithiasis, nephrocalcinosis, polyuria, polydipsia, renal impairment
- Neurological: mental disturbance, fatigue
- Gastrointestinal/abdominal (rare): constipation, peptic ulcer disease, pancreatitis
Optimum use of imaging
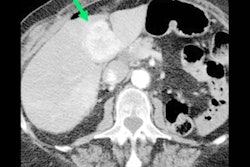
The typical indications for 4D CT, MRI, PET/CT are preoperative localization in indeterminate cases, evaluation of multi-gland disease, persistent/recurrent PHPT following initial surgery, and evaluation of small adenomas.
"Imaging guidelines vary, but all suggest preoperative localization imaging if minimally invasive parathyroidectomy is to be considered, or prior to repeat surgery," the authors noted. "Concordance between two (or more) modalities is often preferred, particularly in cases of persistent/recurrent PHPT."
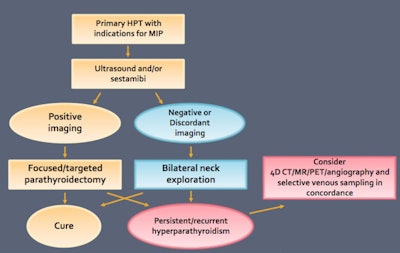 What the imaging guidelines say. NICE guidelines, 2018; Zafereo M et al. Head & Neck, 2019; Wilhelm SM et al. JAMA Surgery, 2016. MIP = minimally invasive parathyroidectomy.
What the imaging guidelines say. NICE guidelines, 2018; Zafereo M et al. Head & Neck, 2019; Wilhelm SM et al. JAMA Surgery, 2016. MIP = minimally invasive parathyroidectomy.For technetium-99m sestamibi, dual-phase protocols work well, using a tracer (sesta-methoxyisobutylisonitrile) with a half-life of six hours and hepatobiliary excretion. Retention of tracer occurs in mitochondria-rich cells, including cardiac myocardium, malignant cells, and oxyphil cells within parathyroid tissue.
"Early tracer uptake is by both the thyroid and parathyroid gland. Differential washout of sestamibi from the thyroid and parathyroid glands is slower in the parathyroid," they pointed out. "Sensitivity is variable, depending on use of planar or hybrid imaging techniques, and is reported as 63% planar, 66% SPECT, and 84% SPECT/CT."
The preferred technique is early and delayed imaging of the neck and mediastinum: early phase planar is 10-15 minutes following tracer administration, delayed phase planar and SPECT is 90-150 minutes after tracer administration, and delayed CT for attenuation correction and anatomical co-registration is recommended. Large field-of-view enables assessment of ectopic tissue and imaging of the neck and mediastinum, including the upper thorax.
Tips and tricks for PET/CT
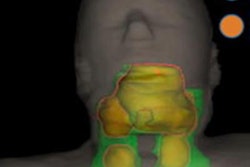
For F-18 fluorocholine PET/CT, the typical appearance is increased tracer uptake relating to a well-circumscribed nodule adjacent to the thyroid, or within the neck or upper mediastinum. Optimizing the PET window settings may help to identify the most accurate focus and thus improve detection of small lesions on the CT component, the Imperial team recommended.
"In [F-18 fluorocholine] PET/CT examinations of the ectopic glands, concordance between second-line imaging is often extremely helpful in cases of unusually located ectopic glands, for preoperative planning, and to minimize risk of morbidity, including scarring and nerve damage," they noted.
Choline uptake can also be seen in inflammation and malignancy, as well as some benign entities such as thymoma and meningioma. Systematic review of the entire study is essential to exclude alternative causes of pathological uptake, they wrote.