Decreased blood supply to the heart muscles, known as cardiac ischemia, can lead to chest pain or even heart attack. Cases of suspected ischemia are currently investigated using invasive coronary angiography (ICA), which provides both anatomical and functional assessment of the coronary vessel. ICA, however, is an invasive procedure that involves relatively rare -- but potentially serious -- risks for patients.
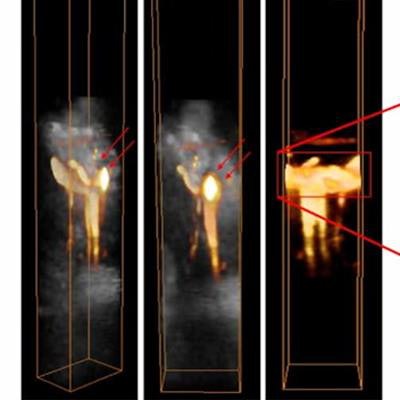
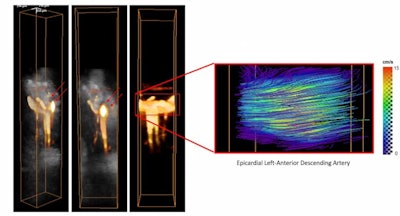 Left: 3D power-Doppler volumes overlaid on anatomical volumes of the myocardium in the left-anterior descending artery. Right: Absolute flow velocities estimated by 4D ultrafast ultrasound flow imaging. All images courtesy of Physics in Medicine and Biology.
Left: 3D power-Doppler volumes overlaid on anatomical volumes of the myocardium in the left-anterior descending artery. Right: Absolute flow velocities estimated by 4D ultrafast ultrasound flow imaging. All images courtesy of Physics in Medicine and Biology.In the peripheral arteries, noninvasive, nonionizing Doppler ultrasound imaging is used instead of angiography. But for cardiac applications, Doppler imaging is difficult because of the rapid motion of the myocardium and the insufficient definition of conventional ultrasound.
To overcome this challenge, researchers at the French research unit Physics for Medicine --the National Institute of Health and Medical Research (INSERM), the City of Paris Industrial Physics and Chemistry Higher Educational Institution (ESPCI Paris), the French National Center for Scientific Research (CNRS), and the University of Paris Science and Letters (PSL University) -- recently introduced a method called ultrafast Doppler coronary angiography (UDCA), which uses 2D ultrafast ultrasound to visualize coronary vessels as small as 100 µm in a beating heart. They have now extended their UDCA approach to three dimensions, enabling 3D imaging and quantification of coronary blood flow in a single heartbeat.
"2D UDCA can quantify relative changes of coronary flow, for example between rest and stress states, but it cannot quantify the absolute coronary flow velocity," explains co-senior author Mathieu Pernot, PhD. "With 3D UDCA, it's a completely different story, as it provides an enormous amount of data at a very high volumetric rate. These data contains all the tissue and flow motion information that allow absolute flow velocity to be measured accurately in a few tens of milliseconds."
In vivo evaluation
To assess their new 3D UDCA technique, Pernot and colleagues performed coronary volumetric blood flow imaging in vivo in open-chest swine experiments. They placed a 32-by-32 element ultrasound matrix-array probe on the animal's left ventricle in the region perfused by the left anterior descending (LAD) artery.
The team designed an ultrafast (1,000 volumes/sec) ultrasound sequence that images the coronary vasculature in 3D using power-Doppler imaging. They also employed vector Doppler analysis (4D ultrafast ultrasound flow imaging) to assess the absolute flow velocities. To estimate flow rates, they first used the 3D power-Doppler volumes to delineate the coronary vessel on 32 successive 2D slices. For each slice, they computed the flow rate by integrating the flux (rate of flow per unit area) over the cross-sectional area of the vessel. Finally, they averaged the flow rate over the different slices.
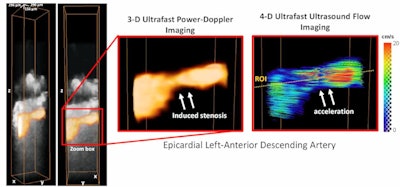 Power-Doppler volumes overlaid on anatomical B-mode volumes show the induced stenosis. 4D ultrafast ultrasound flow imaging (right panel) shows the induced flow acceleration at the centre of the stenosis.
Power-Doppler volumes overlaid on anatomical B-mode volumes show the induced stenosis. 4D ultrafast ultrasound flow imaging (right panel) shows the induced flow acceleration at the centre of the stenosis.In their first set of experiments, the researchers imaged a small portion of the LAD artery in the hearts of five animals. They used 3D UDCA to assess coronary flows throughout the diastolic phase, in which the heart relaxes after contraction, in a single heartbeat.
Arterial flow visualization was most efficient when myocardial tissue motion was small -- at early-diastole before myocardial relaxation and at end-diastole. During the mid-diastole phase, rapid tissue motion prevented accurate signal reconstruction. The researchers also used vector Doppler analysis to assess absolute blood flow velocity. They observed a maximal velocity of approximately 15 cm/sec in the middle of the artery, decreasing towards the edges.
Next, the team examined reactive hyperemia (the increase in blood flow following arterial occlusion) in five animals, after occluding the LAD artery for up to 90 seconds. The maximal flow velocity increased from about 12 cm/sec to more than 20 cm/sec during reactive hyperemia, which corresponded well with the observed flow rate increase from about 70 to 120 ml/min.
The researchers also evaluated whether 3D UDCA can visualize a coronary stenosis (narrowing of the arteries) in three animals. They used an inflatable pneumatic cuff occluder positioned around the artery to create 30%, 50%, and 70% narrowing of the proximal LAD artery.
Overlaying power-Doppler volumes on anatomic volumes of the myocardium revealed a reduced signal in the stenosis region, demonstrating the reduction in the epicardial diameter. Vector Doppler analysis revealed a significant flow acceleration in the center of the stenosis, with maximal velocity of approximately 20 cm/sec.
Comparing flow rates estimated by 3D UDCA with measurements from a gold-standard, invasive coronary flow meter (placed close to the ultrasound probe) revealed good agreement during baseline, reactive hyperemia, and coronary stenosis.
Clinical potential
Writing in Physics in Medicine & Biology on 29 May 2020, the researchers conclude that 3D UDCA could have major potential as a new noninvasive tool to measure coronary flow at the patient's bedside.
"We envision several important clinical applications for diagnosis and management of coronary artery diseases," said Pernot. "One could be estimation of the coronary flow reserve, an important parameter for clinical decision making in coronary intervention that's currently obtained by catheterization under ionizing imaging modalities. Because of its high sensitivity, 3D UDCA could also be used to diagnose coronary microvascular disease, which is challenging with current imaging modalities."
The team is now working to translate 3D UDCA for human use. They note that the open-chest configuration used in this proof-of-concept study provided optimal imaging conditions, while clinical translation will require more challenging transthoracic or transesophageal imaging. Another limitation is the small region that can be imaged, which restricts the field of view to a small part of a large coronary artery.
"We are currently developing new approaches that could image the coronary vasculature of the entire heart," Pernot told Physics World.
Tami Freeman is an online editor for Physics World.
© IOP Publishing Limited. Republished with permission from Physics World, a website that helps scientists working in academic and industrial research stay up to date with the latest breakthroughs in physics and interdisciplinary science.



















