Ultrasound-guided percutaneous microwave ablation is becoming a valuable treatment for benign breast lesions, and skilled interventional radiologists can perfect their technique faster than surgeons can, according to a new study of 755 such lesions published online on 30 April in European Radiology.
"Ultrasound-guided percutaneous microwave ablation is a safe, effective, and feasible technique for minimally invasive treatment of benign breast lesions with good cosmetic outcomes, even for patients with large and high-risk tumors," noted lead author Dr. Qi Yang, from the department of interventional ultrasound at the Chinese PLA General Hospital in Beijing, and colleagues. "It can be mastered easily, and skilled interventional radiologists show a rapid improvement in mastering the technique."
The group's aims were to evaluate the clinical efficacy of microwave ablation (MWA) of benign breast lesions (BBLs) and compare the learning curves of international radiologists and surgeons.
A total of 440 patients with 755 clinicopathologically confirmed BBLs from five centers were prospectively enrolled between February 2014 and July 2018. The team analyzed the technical success, complications, volume reduction ratio (VRR), palpability, and cosmetic satisfaction after ablation. For learning-curve evaluation, they also looked at the ablation time and energy from the number of procedures.
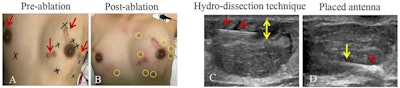 Technical success of microwave ablation (MWA) in a 20-year-old woman with eight fibroadenoma in bilateral breast. Pictured above: A: Appearance of the skin before MWA. Red arrow points to scar from surgery for fibroadenoma before nine months. Black marker indicates location of breast lesions. B: Yellow ring indicates needle site after MWA. C: Needle (red arrows) was inserted into space between lesion margin and skin to infusion of saline, which increased distance (yellow arrow) between lesion and skin. D: Ultrasound shows antenna tip was placed in deepest site of lesion increased echogenicity (red arrow) near irradiating segment of antenna (yellow arrow) at beginning of MWA session. Images courtesy of European Radiology.
Technical success of microwave ablation (MWA) in a 20-year-old woman with eight fibroadenoma in bilateral breast. Pictured above: A: Appearance of the skin before MWA. Red arrow points to scar from surgery for fibroadenoma before nine months. Black marker indicates location of breast lesions. B: Yellow ring indicates needle site after MWA. C: Needle (red arrows) was inserted into space between lesion margin and skin to infusion of saline, which increased distance (yellow arrow) between lesion and skin. D: Ultrasound shows antenna tip was placed in deepest site of lesion increased echogenicity (red arrow) near irradiating segment of antenna (yellow arrow) at beginning of MWA session. Images courtesy of European Radiology.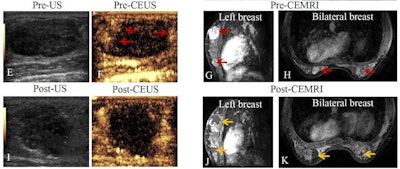 Above (same patient): E: Ultrasound shows hypoechoic lesion before MWA. F: Contrast-enhanced ultrasound shows lesion is hyper-enhancement (red arrow) at margin of lesion in arterial phase. G, H: Transverse contrast-enhanced MRI shows hyperintensity lesion in bilateral breast (arrow) before MWA in arterial phase. Lesion is adjacent to skin and size is 3.9 cm × 2.6 cm × 2.5 cm. I: Contrast-enhanced ultrasound after MWA shows lesion is non-enhancement in arterial phase. J, K: Contrast-enhanced MRI imaging shows hypointensity treatment zone and peripheral nodular enhancement in arterial phase. Volume of lesion decreased at third day after MWA and the size is 3.3 cm × 2.7 cm × 2.5 cm.
Above (same patient): E: Ultrasound shows hypoechoic lesion before MWA. F: Contrast-enhanced ultrasound shows lesion is hyper-enhancement (red arrow) at margin of lesion in arterial phase. G, H: Transverse contrast-enhanced MRI shows hyperintensity lesion in bilateral breast (arrow) before MWA in arterial phase. Lesion is adjacent to skin and size is 3.9 cm × 2.6 cm × 2.5 cm. I: Contrast-enhanced ultrasound after MWA shows lesion is non-enhancement in arterial phase. J, K: Contrast-enhanced MRI imaging shows hypointensity treatment zone and peripheral nodular enhancement in arterial phase. Volume of lesion decreased at third day after MWA and the size is 3.3 cm × 2.7 cm × 2.5 cm.The mean maximum diameter was 1.7 ± 0.6 cm, and about 75% of lesions were < 2 cm in size. The complete ablation rate reached 100%, including 45.8% lesions adjacent to the skin, pectoralis, or areola. After a median follow-up of 13.7 months, the 12-month VRR of all lesions was 98%, and for 1- to 2-cm and ≥ 2-cm lesions it was 98.6% and 97%, respectively.
Around 56% of BBLs became nonpalpable (palpable in 85.7% of cases before MWA) by both the clinician and patient. Also, the cosmetic and minimally invasive satisfaction rates were good or excellent in 98.4% and 94.5% of patients, respectively.
The median ablation time/cm3 and energy/cm3 decreased as experience increased, the authors explained. The energy/cm3 of the interventional radiologist with five years of experience was lower than that of the interventional radiologist with one year of experience as well as the surgeons, while the ablation time/cm3 of surgeons was comparable with that of the interventional radiologist with five years of experience at relatively mature phase.
"These findings indicate that the interventional radiologist with richer experience had more comprehensive abilities in ultrasound imaging, thermal field management, and puncture technique," the authors noted. "Therefore, the higher skill level of this interventional radiologist shortened the ablation time and decreased the energy and complications."
Interventional radiologists can master the BBL ablation technique faster than surgeons can, they emphasized.
The main limitation of the study is the relatively small number of patients with ≥ 2 cm BBLs. This was because 77.2% (583/755) of BLLs were diagnosed as fibroadenomas in the study, while fibroadenomas are usually < 3 cm in diameter on clinical examination. Another limitation is the relatively short median follow-up of 13.7 months, and the authors conceded that a longer follow-up period is warranted to evaluate the long-term volume reduction rate for BBLs.
A further randomized controlled study is needed to compare the treatment efficacy with those of other therapeutic options, they concluded.