A normal brain F-18 FDG-PET scan can help rule out the short-term risk of dementia in older patients who present to memory clinics with cognitive complaints, according to a study published on 13 August in Alzheimer's Research and Therapy.
French researchers analyzed images from a large group of patients referred for scans at a memory clinic and found that the PET scans showed a high negative predictive value (NPV) for predicting which patients developed dementia.
“Brain F-18 FDG PET scans can rule out the risk of dementia conversion early with high certainty, allowing better customization of patient management regimens in the short term,” wrote Dr. Sébastien Heyer of the University of Lorraine, Nancy, and colleagues.
Neurodegenerative diseases such as Alzheimer’s disease are a major public health problem, resulting in a loss of autonomy for many patients as well as generating significant costs (estimated at €736 billion globally in 2015) for diagnosis and management of patients, the authors explained.
That's why identifying patients who will convert to dementia is essential for establishing management regimens early and developing future therapeutics, they added.
While F-18 FDG-PET scans have been shown to predict the progression from mild cognitive impairment to Alzheimer’s dementia, there is currently a lack of large longitudinal studies under real-life conditions to establish its value for predicting the risk of dementia in undiagnosed patients, the researchers noted.
To address this knowledge gap, the group culled images of 403 patients with no diagnosis of dementia at the time they were referred to their memory clinic. All patients presented with cognitive complaints and underwent MRI scans before the F-18 FDG-PET scans and were followed for at least three years.
According to combined visual and semiquantitative analyses, of the 403 patients, 120 (30%) had normal brain F-18 FDG PET scans; two (< 1%) were abnormal but incompatible with a neurodegenerative disease, and 281 (70%) were classified as neurodegenerative.
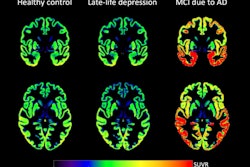
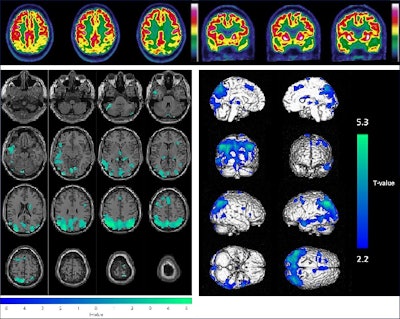 Example of the combined visual (upper panel, axial and coronal slices of brain F-18 FDG-PET images) and semiquantitative (lower panel, with hypometabolisms in green projected on axial MRI slices on the left and hypometabolisms in blue on a 3D volume rendered on the right) analysis for a 65-year-old male patient (initially diagnosed with mild cognitive impairment); these results were consistent with Alzheimer’s disease. The final diagnosis was Alzheimer’s disease and conversion to dementia after 31.5 months.Image and caption courtesy of Alzheimer's Research and Therapy.
Example of the combined visual (upper panel, axial and coronal slices of brain F-18 FDG-PET images) and semiquantitative (lower panel, with hypometabolisms in green projected on axial MRI slices on the left and hypometabolisms in blue on a 3D volume rendered on the right) analysis for a 65-year-old male patient (initially diagnosed with mild cognitive impairment); these results were consistent with Alzheimer’s disease. The final diagnosis was Alzheimer’s disease and conversion to dementia after 31.5 months.Image and caption courtesy of Alzheimer's Research and Therapy.
Within three years, 105 (26%) patients converted to dementia, and 12 (3%) of these died; 52 (13%) died without any dementia conversion; and 246 (61%) were still alive and did not experience any dementia conversion.
Based on these results, the authors calculated that the F-18 FDG-PET scans had a negative predictive value of 85% for predicting which patients developed dementia.
“Brain F-18 FDG-PET, depending on its different availabilities across countries and local/national recommendations, could thus be a useful complementary investigation for assessing cognitive complaints,” the group wrote.
Ultimately, from a diagnostic or therapeutic perspective, the use of cerebral spine fluid biomarkers, amyloid or tau PET scans, and recently developed plasma biomarkers remain key for diagnosing neurodegenerative diseases, the researchers wrote.
But early F-18 FDG-PET imaging of the brain could serve as an adjunct examination to these techniques and could even be suitable on its own in areas where such advanced and costly resources might not be available, they noted.
“Additional multicentric studies pairing PET imaging data with patient data collected at a longer interval from the scan (e.g., 5 or 10 years) to further verify the prognostic value of brain PET studies in predicting the conversion to dementia could be implemented,” the group concluded.
The full study is available here.