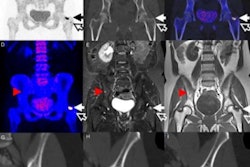
Ultrasound can be used to release nerve-blocking agents contained in liposomes and relieve patients from pain. This would be an alternative to opioids and open up the possibility of a safer, on-demand, and personalized management of pain.
Opioids are frequently prescribed to patients in an attempt to relieve disease- or surgery-related pain. But such drugs carry a high risk of addiction and overdose that can potentially lead to death. This became a cause of concern over the past decade as official figures revealed an increase in deaths by pain-reliever overdose in the U.S. of more than 400% in women and 237% in men between 1999 and 2010.
In response to this problem, researchers from Boston, Madrid, and Hong Kong teamed up to create a safer substitute that would provide instant pain relief at specific locations. They designed a system that uses engineered liposomes containing an anesthetic agent, and whose outer shell is triggered by ultrasound to burst the liposome open and release its cargo. This strategy provides local anesthesia where needed (Nature Biomedical Engineering, 9 August 2017, Vol. 1, pp. 644-653).
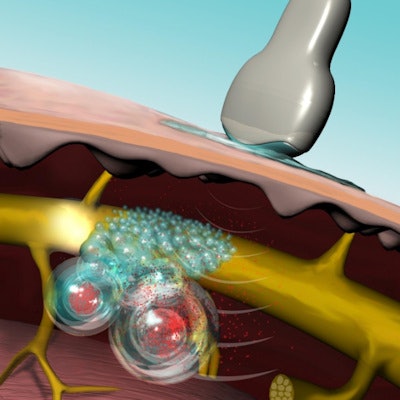
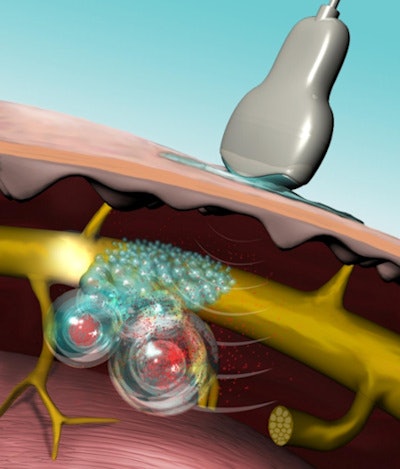 Ultrasound interacts with the protoporphyrin IX contained in the bilayer to burst the liposome open and release the anesthetic TTX. Image courtesy of Mary O'Reilly.
Ultrasound interacts with the protoporphyrin IX contained in the bilayer to burst the liposome open and release the anesthetic TTX. Image courtesy of Mary O'Reilly.Sono-sensitive drug-delivery system
Ultrasound has been investigated to direct diverse organic vehicles to specific locations. For example, microbubble-induced opening of the blood-brain barrier has reached the human trial stage. The noninvasive and nonionizing nature of ultrasound makes it a suitable energy source to direct these vehicles, but it is its extended depth of penetration that makes ultrasound the trigger of choice over other techniques such as near-infrared light.
Of all the existing vehicles, liposomes -- spherical vesicles with a lipid bilayer shell -- were preferred due to their customizable potential and ability to carry tetrodotoxin (TTX), a molecule administered in clinical trials to attenuate cancer pain. FDA-approved protoporphyrin IX (PPIX) was encapsulated between the two layers of the liposome and used as a sonosensitizer to trigger the release of the anesthetic under the action of the ultrasound energy. The team investigated various combinations of frequencies, intensity, duration, and duty cycle of insonation to ensure maximum efficiency in the release of TTX.
The researchers conducted experiments in rats to validate the need for PPIX and verify whether TTX was responsible for nerve blockade -- the phenomenon responsible for anesthesia. They injected liposomes directly in the nerve and sonicated, while assessing the status of the nerve by timing how long the rat could stay on a hot plate. The results validated their hypotheses and the group observed the duration and intensity of anesthesia were dependent upon the duration and intensity of the ultrasound beam.
After one injection, a 10-minute insonation led to 34 hours of nerve blockade; subsequent insonations with no reinjection of liposomes led to around 1 hour of additional nerve blockade. This result paves the way for personalized narcotic-free pain management. The technique also proved to be safe, as all 20 animals used in the experiments with TTX and PPIX survived.
 Alina Rwei (left) and Juan Paris (center) described how ultrasound could be used to trigger local anesthesia. Daniel Kohane (right) was the senior author of the study.
Alina Rwei (left) and Juan Paris (center) described how ultrasound could be used to trigger local anesthesia. Daniel Kohane (right) was the senior author of the study.The future of pain management?
These results are very promising. The fact the degree of nerve blockade is controlled by the ultrasound duration and intensity allows for customizable pain management. Patients could receive an injection at the hospital and relieve their pain themselves at home, whenever they need, using a small portable ultrasound device. This could potentially help combat opioid addiction, reduce the overall duration of hospitalization and hence alleviate bed blocking.
Samuel Vennin is a doctoral student contributor to medicalphysicsweb, working in cardiovascular medicine and numerical modeling at King's College London. He is studying the hemodynamic mechanisms behind cardiovascular diseases and the relationship between blood flow and pressure to derive new clinical protocols.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.