Integrating an AI tool for colorectal polyp classification in CT colonography can help to improve radiologists' therapy recommendations, German researchers have reported in an article posted on 25 January by European Radiology.
"AI-based characterization beyond the size and morphology of colorectal polyps at CT colonography as a second reader might enable a more precise selection of polyps eligible for subsequent endoscopic resection," noted first author Dr. Sergio Grosu, a radiologist at the Grosshadern Campus, LMU University Hospital, Munich, and colleagues, adding that adenomatous colorectal polyps require endoscopic resection, as opposed to nonadenomatous hyperplastic colorectal polyps.
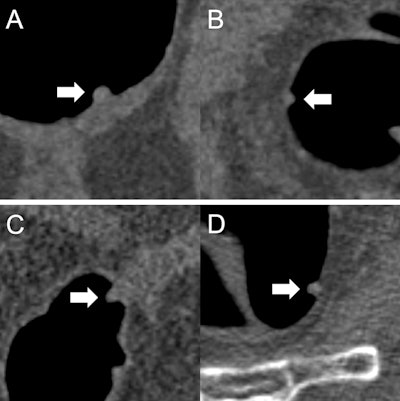 (A) A 9 mm tubular adenoma that was classified by all readers as "polypectomy: yes." The initial recommendation was confirmed based on the prediction "adenomatous" of the AI model. (B) A 6 mm hyperplastic polyp that was classified by all readers as "polypectomy: no." The initial recommendation was confirmed based on the prediction "nonadenomatous" of the AI model. (C) An 8 mm tubular adenoma that was classified by three readers as "polypectomy: no." The initial recommendation was corrected by all three readers based on the prediction "adenomatous" of the AI model. (D) A 7 mm hyperplastic polyp that was classified by two readers as "polypectomy: yes." The initial recommendation was corrected by both readers based on the prediction "nonadenomatous" of the AI model. All figures courtesy of Dr. Sergio Grosu et al and European Radiology.
(A) A 9 mm tubular adenoma that was classified by all readers as "polypectomy: yes." The initial recommendation was confirmed based on the prediction "adenomatous" of the AI model. (B) A 6 mm hyperplastic polyp that was classified by all readers as "polypectomy: no." The initial recommendation was confirmed based on the prediction "nonadenomatous" of the AI model. (C) An 8 mm tubular adenoma that was classified by three readers as "polypectomy: no." The initial recommendation was corrected by all three readers based on the prediction "adenomatous" of the AI model. (D) A 7 mm hyperplastic polyp that was classified by two readers as "polypectomy: yes." The initial recommendation was corrected by both readers based on the prediction "nonadenomatous" of the AI model. All figures courtesy of Dr. Sergio Grosu et al and European Radiology.
The current lack of data on the impact of computer-aided classification of CT colonography-detected colorectal polyps on therapy management prompted the Munich group to evaluate the effect of AI-assisted differentiation of nonadenomatous and adenomatous colorectal polyps at CT colonography on radiologists' therapy management using a radiomics-based machine-learning model analyzing polyp characteristics beyond size and morphology.
Their CT colonography images were acquired with varying scanning protocols on multiple CT scanners from several vendors (Canon Medical Systems, GE Healthcare Systems, Philips Healthcare, Siemens Healthineers). Only polyps with available histopathologic reports were included in the study.
Five board-certified radiologists evaluated CT colonography images with colorectal polyps of all sizes and morphologies retrospectively and decided whether the depicted polyps required endoscopic resection. After a primary unassisted reading based on current guidelines, a second reading with access to the classification of a radiomics-based, random-forest AI-model labeling each polyp as "nonadenomatous" or "adenomatous" was performed. Performance was evaluated using polyp histopathology as the reference standard.
A total of 77 polyps in 59 patients comprising 118 polyp image series (47% supine position, 53% prone position) were evaluated unassisted and AI-assisted by the radiologists, resulting in a total of 1,180 readings (subsequent polypectomy: yes or no), according to the authors.
In unassisted readings, radiologists achieved an accuracy of 76% (standard deviation [SD] = 1%), a sensitivity of 78% (SD = 6%), and a specificity of 73% (SD = 8%) on average on selecting polyps eligible for polypectomy. In AI-assisted readings, radiologists achieved an accuracy of 84% (SD = 1%), a sensitivity of 85% (SD = 1%), and a specificity of 82% (SD = 2%) in selecting polyps eligible for polypectomy.
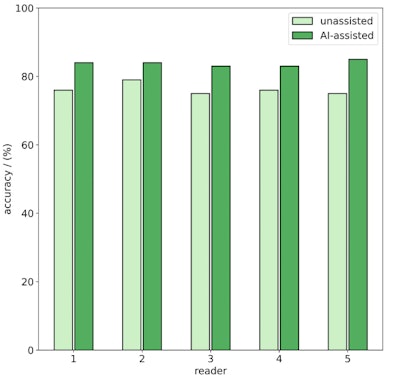 Comparison of reading accuracy in the selection of colorectal polyps on CT colonography that are eligible for subsequent endoscopic resection for unassisted (light green) and AI-assisted readings (dark green).
Comparison of reading accuracy in the selection of colorectal polyps on CT colonography that are eligible for subsequent endoscopic resection for unassisted (light green) and AI-assisted readings (dark green).
The machine-learning model alone achieved an accuracy of 83%, a sensitivity of 82%, and a specificity of 85% in selecting polyps eligible for polypectomy. The difference between unassisted and AI-assisted reading results was significant (p < 0.001). Interreader agreement between the five radiologists was Fleiss' kappa 0.69 (0 = no agreement, 1 = full agreement) in unassisted readings and Fleiss' kappa 0.92 in AI-assisted readings.
The researchers found that 66 reading decisions were changed in the AI-assisted reading compared with the unassisted reading. Each reader changed 13.2 (SD = 1.9) decisions on average. In total, the changed decision was correct according to the histopathological reference standard in 55/66 (83%) cases and false in 11/66 (17%) cases. For polyps ≤ 5 mm, no decision was changed. For polyps of 6 mm to 9 mm, the changed decision was correct in 47/54 (87%) cases and false in 7/54 (13%) cases. For polyps ≥ 10 mm, the changed decision was correct in 8/12 (67%) cases and false in 4/12 (33%) cases.
"Compared with unassisted reading, AI-assisted reading had higher accuracy, sensitivity, and specificity in selecting polyps eligible for polypectomy," they wrote. "This study indicates that integrating an AI tool for colorectal polyp classification in CT colonography could further improve radiologists' therapy management. However, further studies are needed to confirm this finding and histopathologic polyp evaluation is still mandatory."
Implementation of AI tool
The authors think this is the first study evaluating the impact of AI-based polyp classification in CT colonography on radiologists' therapy management. The AI model performed well, but its impact on radiologists in a clinical scenario has not yet been tested, Grosu told AuntMinnieEurope.com on 28 January.
"Even a well-functioning model is useless if it does not add value to radiologists' clinical decision-making," he said. "We were very pleased to see that integrating our AI model for colorectal polyp classification in CT colonography could further improve radiologists' therapy management, but we are still at too early a stage of development to implement our AI model in routine clinical practice. However, this is a goal for the future."
The researchers are currently planning a follow-up project, and they hope to be ready to present their further results at ECR 2026.
You can read the full European Radiology article here.