Appropriate use of spectral CT can help to shine a light in challenging abdominal and pelvic cases and have a positive impact on patient care by changing management decisions, Spanish researchers have reported in a prize-winning study.
Spectral CT is useful for problem-solving, and the radiologist can aid in successful decision-making and avoid additional imaging or procedures, but it's important to keep aware of the limitations of spectral CT, according to Dr. Ana Villanueva Campos and colleagues from the Servicio de Radiodiagnóstico at Hospital Universitario Ramón y Cajal in Madrid.
 A 43-year-old man with right renal colic. (A) Conventional image shows a large stone in the right renal pelvis of indeterminate composition. (B, C) Spectral images confirm the presence of a uric acid stone. This is clinically relevant as uric acid calculi can be treated medically (urinary alkalinization), whereas other calculi (calcium, etc.) may require interventional procedures (stone removal or external shock wave lithotripsy). All figures courtesy of Dr. Ana Villanueva Campos et al and presented at RSNA 2023.
A 43-year-old man with right renal colic. (A) Conventional image shows a large stone in the right renal pelvis of indeterminate composition. (B, C) Spectral images confirm the presence of a uric acid stone. This is clinically relevant as uric acid calculi can be treated medically (urinary alkalinization), whereas other calculi (calcium, etc.) may require interventional procedures (stone removal or external shock wave lithotripsy). All figures courtesy of Dr. Ana Villanueva Campos et al and presented at RSNA 2023.
Spectral CT – or dual energy CT (DECT) – was introduced clinically in 2006. It involves acquisition of high- and low-energy x-ray attenuation data. Different types of scanners are available on the market, and they can be source-based (one or two tubes, also known as double source) or detector-based (dual-layer detector).
"Additional info is obtained because different types of materials and tissues may attenuate x-rays differently at different energies, depending on their elemental composition," the Madrid researchers wrote in a poster exhibit that received a certificate of merit award at the RSNA meeting. "Different spectral maps are available."
By using virtual monoenergetic images at low energy level values (45 keV), hypervascular tumors such as hepatocellular carcinoma will be highlighted due to iodine boost expected from the photoelectric effect. The technology can lead to better detection of lesions -- "it helps you in diagnosing" -- and improved assessment of viable tumor or recurrence versus post-treatment changes, they noted.
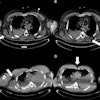
 An 85-year-old man with previous rectal tumor and abdominoperineal excision of the rectum had a follow-up CT exam. (A) Conventional image shows an indeterminate soft tissue lesion at the anastomotic site that is barely visible. Virtual low keV monoenergetic image (B) and Z-effective (C) improve detection of this enhancing mass compared to conventional image. (D) Spectral map such as iodine no water also makes it possible to quantify the iodine uptake, which was 1.3 mg per mL in this case. All these findings were in keeping with local tumoral recurrence in the anastomotic site.
An 85-year-old man with previous rectal tumor and abdominoperineal excision of the rectum had a follow-up CT exam. (A) Conventional image shows an indeterminate soft tissue lesion at the anastomotic site that is barely visible. Virtual low keV monoenergetic image (B) and Z-effective (C) improve detection of this enhancing mass compared to conventional image. (D) Spectral map such as iodine no water also makes it possible to quantify the iodine uptake, which was 1.3 mg per mL in this case. All these findings were in keeping with local tumoral recurrence in the anastomotic site.
"Virtual monochromatic images (VMIs) simulate the appearance of images obtained with a monochromatic x-ray source. They are generated by a process equivalent to that of the decomposition of materials using the contribution of the photoeclectic and Compton effect," they explained. "In practice, systems offer a wide range of energy levels, from 35 to 200 keV according to the DECT platform. At low energy level values (40 to 70 keV), there is an iodine boost expected from the photoelectric effect."
Remember that at low energy level values, there is an iodine boost expected from the photoelectric effect (tumoral thrombus), whereas bland thrombus shows a flat curve, according to the authors. There are discrepancies in the optimal threshold for thrombus iodine uptake identification; studies show it is around 1 mg per mL.
"Low-keV virtual monoenergetic image reconstruction and iodine overlay images improve assessment of wall enhancement, enabling better evaluation of gallbladder wall hyperemia in cases of acute cholecystitis, as well as accentuating regional hepatic parenchymal hyperemia," they pointed out. "These techniques also improve detection of gallbladder wall gangrene or perforation by depiction of areas of decreased enhancement in cases of complicated cholecystitis or gallbladder volvulus."
 A 61-year-old man with colorectal cancer had a routine CT follow-up exam. (A) Conventional image shows incidental finding of gallbladder wall thickening with heterogeneous enhancement of its wall and mild inflammatory changes suspicious of cholecystitis. Spectral maps: iodine overlay map (B), low keV virtual monoenergetic (C), and Z-effective (D). All spectral images improve the assessment of wall enhancement and complications, such as perforation (arrows).
A 61-year-old man with colorectal cancer had a routine CT follow-up exam. (A) Conventional image shows incidental finding of gallbladder wall thickening with heterogeneous enhancement of its wall and mild inflammatory changes suspicious of cholecystitis. Spectral maps: iodine overlay map (B), low keV virtual monoenergetic (C), and Z-effective (D). All spectral images improve the assessment of wall enhancement and complications, such as perforation (arrows).
Using low monoenergetic maps (ex: 45 keV), radiologists can better assess the vessels and therefore the presence of complications such as pseudoaneurysm and thrombosis, the authors continued. "Virtual non contrast images may also be helpful for detection of hemorrhage as a possible complication of acute pancreatitis (it remains hyperdense on VNC)."
Spectral CT also improves sensitivity in detection of prostatic lesions; qualitative and quantitative depiction of contrast medium uptake can be evaluated. "Use virtual monoenergetic images at low energy to assess the prostate in your clinical practice and try to train your eye to detect prostate tumors. In our experience, incidental prostate cancer found in spectral CT is not rare. Further studies are needed to differentiate cancer from benign prostatic hyperplasia (BPH)," they pointed out.
There is relatively little information in the literature about the role of spectral CT in gynecological tumors, specifically in vulva cancer. "Our experience is that low-energy VMIs along with other reconstruction methods significantly improve tumor detection."
The co-authors of this exhibit were Drs. Elena Canales Lachén, Raquel García Latorre, and Nicolas Almeida Arostegui.