Researchers from Ireland have used data from dual-energy x-ray absorptiometry scans to estimate the country's prevalence of osteoporosis. Their findings have highlighted an urgent need to establish a national program to reduce the illness burden.
"We have shown for the first time in a large Irish population that low bone mass defined by [dual-energy x-ray absorptiometry, DEXA/DXA] classification is common in men and women aged ≥ 50 years, whether they have risk factors or not, or previous osteoporotic fractures," noted lead author Prof. John Carey, professor in rheumatology at the National University of Ireland and clinical lead in DXA, osteoporosis, and fracture liaison services at Galway University Hospitals.
Ireland has one of the largest proportional illness burdens related to osteoporosis in Europe, and it is projected to have the greatest increase over the coming decade, Carey and his colleagues wrote in an article published on 10 August in JBMR Plus.. Moreover, the cost of managing those who fracture will double by 2030.
DEXA-measured bone mineral density (BMD) is an established criteria to help understand the epidemiology of osteoporosis and identify those at risk for fracture. In this study, the researchers estimated prevalence in Ireland based on DEXA metrics identified in men and women who had scans between January 2000 and November 2018 as part of an ongoing epidemiological study.
A total of 33,344 subjects met the study's inclusion criteria. Among the cohort, the authors compared the prevalence of DEXA low bone mass (T-score < -1.0) and of osteoporosis (T-score ≤ -2.5) in adults without major risk factors or fractures, with one or more major risk factors, and with one or more major osteoporotic fractures.
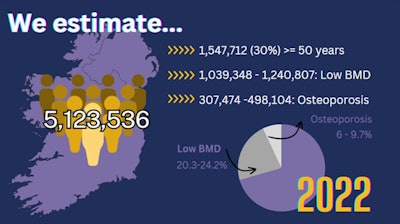 A graphic showing the situation facing Irish healthcare professionals. Image courtesy of JBMR Plus.
A graphic showing the situation facing Irish healthcare professionals. Image courtesy of JBMR Plus.According to the findings, more than one-half of the men and women without fractures had low bone mass (T-score < -1.0) at one or more skeletal sites, whereas almost one in five had osteoporosis (T-score ≤ -2.5) at one or more skeletal sites. The majority of those with a previous major osteoporotic fracture had low bone mass, whereas only one in three had a T-score less than or equal to -2.5.
Applying these results to Ireland's 2022 census figure of approximately 5.1 million people, the researchers estimated that between 1 million men and 1.2 million women over 50 years old have low bone mass, whereas between 308,474 men and 498,104 women have osteoporosis.
"We describe for the first time a reasonable estimate of the true prevalence of low bone mass and osteoporosis in a large cohort of older Irish adults using Irish data," Carey and colleagues.
Ultimately, the study highlights that DEXA-measured BMD remains an appropriate choice for clinicians to diagnose osteoporosis in perimenopausal or postmenopausal women, or men ages 50 and older without a major osteoporotic fracture, the researchers noted. Future projects will assess the validity of various fracture risk tools, they added.
"These data are important for the diagnosis of osteoporosis in clinical practice, and national policy to reduce the illness burden of osteoporosis," the authors concluded.
The full article can be found here.



















