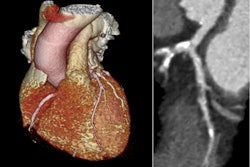
Coronary artery calcification is a marker of cardiovascular risk, but what is its association with qualitatively and quantitatively assessed plaque subtypes? In its most recent post-hoc analysis, the Scottish CT of the Heart (SCOT-HEART) trial research team assessed CT images and five-year clinical outcomes in participants and discovered that calcium score is an imperfect prognostic measure, confirming current testing strategy guidelines which advocate the use of coronary CT angiography (CCTA) for quantitative assessment rather than calcium score for symptomatic patients.
"We did this study because the overlap between coronary artery calcification and other types of coronary artery plaque was important to understand in more detail," corresponding author Dr. Michelle Williams, PhD, senior radiology lecturer from the University of Edinburgh told AuntMinnieEurope.com.
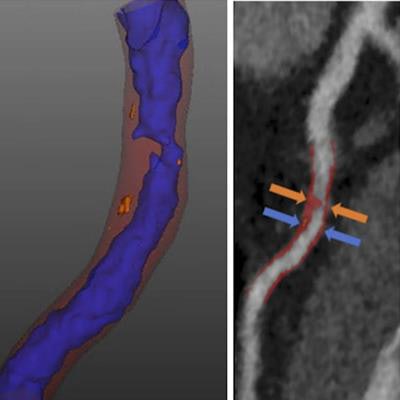
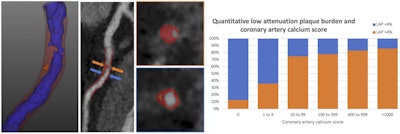 (Left) CTA plaque analysis showing lumen in blue, noncalcified plaque in red and low-attenuation plaque (LAP) in orange. (Right) LAP increases as the calcium score increases but is common in symptomatic patients with zero or low calcium score. All images courtesy of SCOT-HEART trial.
(Left) CTA plaque analysis showing lumen in blue, noncalcified plaque in red and low-attenuation plaque (LAP) in orange. (Right) LAP increases as the calcium score increases but is common in symptomatic patients with zero or low calcium score. All images courtesy of SCOT-HEART trial."Quantitative assessment of coronary artery plaque provides the most robust and comprehensive assessment of plaque subtypes throughout the coronary artery tree. In particular, we were able to assess the highest risk plaque sub-type, the low-attenuation noncalcified plaque," she added.
In their article published online on 16 September in the European Heart Journal -- Cardiovascular Imaging, the authors from the University of Edinburgh and Cedars-Sinai Medical Centre, Los Angeles, aimed to determine the presence of visually and quantitatively assessed adverse plaques in patients across the range of coronary artery calcium scores and correlate this with subsequent clinical events.
The team measured Agatston coronary artery calcium score (CACS) on noncontrast CT in 1,769 patients, and the score was stratified as zero (0 Agatston units, AU), minimal (1-9 AU), low (10-99 AU), moderate (100-399 AU), high (400-999 AU), and very high (≥ 1000 AU). The group investigated adverse plaques by qualitative (visual categorization of positive remodelling, low-attenuation plaque, spotty calcification, and napkin ring sign) and quantitative (calcified, noncalcified, low-attenuation, and total plaque burden; Autoplaque) assessments.
Assessment results
Of 1,769 patients, 36% had a zero, 9% minimal, 20% low, 17% moderate, 10% high, and 8% very high CACS. Amongst patients with a zero CACS, in the visual assessment of coronary plaque characteristics, 14% had non-obstructive disease, 2% had obstructive disease, 2% had visually assessed adverse plaques, and 13% had low-attenuation plaque burden lower than 4%. Furthermore, noncalcified and low-attenuation plaque burden increased between patients with zero, minimal, and low CACS (P < 0.001), but there was no statistically significant difference between those with medium, high, and very high CACS, they stated.
In terms of clinical outcomes, of the 41 patients in whom myocardial infarction occurred, 10% had zero CACS. The authors noted that CACS greater than 1,000 AU and low-attenuation plaque burden were the only predictors of myocardial infarction, independent of obstructive disease, and 10-year cardiovascular risk score.
 Team members from the University of Edinburgh (left to right): Edwin van Beek, David Newby, Julian Sparrow, Barbara Allen, David Brian, Scott Semple, Michelle Williams, Amanda Hunter, and Nick Weir.
Team members from the University of Edinburgh (left to right): Edwin van Beek, David Newby, Julian Sparrow, Barbara Allen, David Brian, Scott Semple, Michelle Williams, Amanda Hunter, and Nick Weir.The authors noted that in patients with stable chest pain, zero CACS is associated with a good but not perfect prognosis, and CACS cannot rule out obstructive coronary artery disease, non-obstructive plaque, or adverse plaque phenotypes, including low-attenuation plaque.
"In the 1,769 symptomatic patients that had CT as part of the SCOT-HEART trial, we found that looking at coronary artery calcium score alone cannot rule out the presence of coronary artery disease, or high-risk disease such as obstructive stenoses or low-attenuation plaque," said Williams, who is also a consultant radiologist and president elect of the British Society of Cardiovascular Imaging. She suggests that patients with symptoms should be assessed with CCTA.
An important question remains about how best to identify and treat coronary artery disease in asymptomatic individuals, according to Williams. For that reason, the university is currently recruiting participants for the SCOT-HEART 2 trial led by Prof. David Newby, from the Centre of Cardiovascular Science in Edinburgh. Recruitment opened in January 2020, and the plan is to involve at least 6,000 subjects. A team from Western General Hospital Edinburgh is responsible for the recruitment process, while scanning is being performed at Royal Infirmary Edinburgh.
 SCOT-HEART 2 is funded until 2027 by the British Heart Foundation.
SCOT-HEART 2 is funded until 2027 by the British Heart Foundation."The SCOT-HEART 2 trial will recruit patients who are at risk of heart disease and randomize them to have either the current standard of care assessment with a cardiovascular risk score or to have CT coronary angiography. We hope this will help us identify whether management based on CT coronary angiography improves treatment and outcomes for at-risk asymptomatic individuals," she said.
SCOT-HEART is a multicenter open-label parallel-group randomized controlled trial that assessed the use of CT in patients who attended the outpatient department with suspected angina pectoris secondary to coronary artery disease. It recruited 4,146 patients between 18 and 75 years old who attended cardiology outpatient clinics at 12 sites and were randomized to either standard care or standard care plus CT. In the intervention arm, 1,778 of the 2,073 participants underwent CT, of which 1,769 images were available and of suitable image quality for analysis.
The team won the Scientific Paper of the Year award in the inaugural EuroMinnies scheme in 2019.