A new study from Lyon, France, has shown that chest CT is a rapid and adequately reliable tool for referring patients requiring hospitalization to the COVID-19-positive (COVID+) or COVID-19-negative (COVID−) hospital units when response times for virological tests are unacceptably long. The findings were published online in European Radiology on 19 August.
The authors, led by a team from the radiology department of university hospital Hospices Civils de Lyon (HCL), are convinced that using CT to triage patients suspected of being infected with COVID-19 could help orientate them quicker to dedicated units and avoid congestion on the emergency ward.
Their study involved 694 consecutive patients across three Lyon-based HCL emergency departments (Hospital Croix-Rousse, Hospital Edouard Herriot, Hospital Lyon Sud) between 3 March and 4 April for whom hospitalization was planned for either COVID-19-negative or non-COVID-related reasons. These patients underwent a chest CT and one or several reverse transcription polymerase chain reaction (RT-PCR) tests.
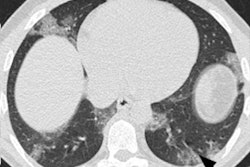
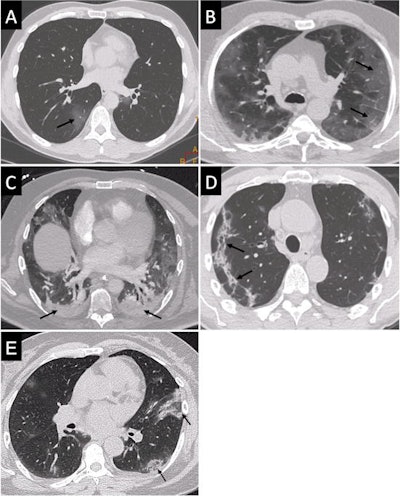 Typical images from five different patients who were COVID-19 positive on a virology test: ground-glass opacity (A), crazy paving (B), posterior lung consolidations (C), subpleural bands of consolidations (D), and reversed halo sign (E). Images courtesy of European Radiology.
Typical images from five different patients who were COVID-19 positive on a virology test: ground-glass opacity (A), crazy paving (B), posterior lung consolidations (C), subpleural bands of consolidations (D), and reversed halo sign (E). Images courtesy of European Radiology.All CT examinations were read by experienced HCL radiologists, who categorized cases as "Surely COVID+," "Possible COVID+," and "COVID−".
Readers rated chest CTs as "Surely COVID+," when patients presented with peripheral, bilateral, or multifocal ground-glass opacity (GGO) of rounded morphology and/or consolidation or crazy paving, reversed halo sign, or subpleural bands of consolidations. They classed scans as "Possible COVID+," when they had multifocal, diffuse, peripheral, or unilateral GGO and/or consolidation lacking a specific distribution or showed only few very small GGO with a nonrounded and nonperipheral distribution or when there were atypical findings, such as large pleural effusion, major lymph node size increase, or bronchiolitis pattern. Scans were deemed "COVID−" when the chest CT was normal or demonstrated another pathology.
The team calculated sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) using the final RT-PCR test as standard of reference. In a further step, the delays for CT reports and RT-PCR results were recorded and compared.
Sensitivity and specificity
Among the 694 patients, 287 were positive on the final RT-PCR exam. From the 694 chest CTs, 308 were rated as "Surely COVID+", 34 as "Possible COVID+," and 352 as "COVID−." When considering only the "Surely COVID+" CT as positive (the other two classes being deemed negative), accuracy, sensitivity, specificity, PPV, and NPV reached 88.9%, 90.2%, 88%, 84.1%, and 92.7%, respectively, with respect to the final RT-PCR test. Agreement between the two methods was good, with a kappa of 0.77 (95% confidence interval [CI] 0.73-0.82).
Furthermore, when considering the "Surely COVID+" and "Possible COVID+" classes as positive CT and "COVID−" class as negative, chest CT accuracy was calculated at 86.6%, sensitivity at 93.4%, specificity at 81.8%, PPV at 78.4%, and NPV at 94.6%. Agreement between the two methods was good, with a kappa of 0.73 (95% CI 0.68-0.78)
While pulmonary and otolaryngology symptomatology was the main reason for admission at the emergency department for 67% of the 694 patients, 124 individuals (17.9%) were fully asymptomatic to COVID common signs, from which 21 (17%) had RT-PCR positive tests. The rate of RT-PCR positive tests varied with regard to the reason for admission and was relatively high even for non-COVID-19-related symptoms such as trauma or psychiatric disorders, highlighting the need for speedy orientation even in asymptomatic patients or those admitted for other reasons.
Speed of reporting
The researchers also showed that CT reporting was faster than RT-PCR test reporting. The mean delay for CT reports was three times shorter than for RT-PCR results (187 ± 148 minutes versus 573 ± 327 minutes, p < 0.0001). They noted that interreader reproducibility was very good with a kappa of 0.86.
"Even if real-time RT-PCR is the fastest available viral detection method, chest CT clearly outperforms the RT-PCR in terms of delay to report the presence of COVID-19 infection. In our study, the delay between the request by the emergency department and the validation of the report was three times longer for the virological test than for chest CT," the authors wrote.
They stated that in the "Surely COVID+" scans, chest CT accuracy reached 88.9% with a sensitivity and specificity of 90.2% and 88%, respectively, making it a reliable tool to use for triage. Factoring in the difference in reporting delays and the NPV and PPV values, the authors urged the use of the chest CT to orient patients. In the current epidemic phase, suspected positive patients could then wait in an isolated room in the COVID+ unit for the final virological test result.
"As the NPV is not equal to 100%, we consider that the probability of orienting a positive patient toward the COVID− unit is high and the risk of contaminating other patients is important. As a result, for patients that are negative according to chest CT, we suggest that they wait in the emergency department until the results of the virological test are available and then be oriented toward the COVID− or COVID+ units accordingly," the researchers said.
The scanning parameters included a mean tube voltage of 119.3 ± 11.9 kVp (range: 80-140 kVp), and mean slice thickness of 2.3 ± 0.8 mm (range: 0.6-3 mm). Mean volumetric computed tomography dose index (CTDIvol) and mean dose length product (DLP) were 9.71 ± 4.39 mGy (range: 2.8-33.9 mGy) and 387.4 ± 223.6 mGy-cm (range: 104.9-1903 mGy-cm), respectively.
Structured reports
In other news, an Italian team has released a consensus document about structured reporting of chest CT in COVID-19 pneumonia.
"The proposed structured report could be of help both for expert radiologists and for the less experienced who are faced with the management of these patients," noted lead author Prof. Dr. Emanuele Neri, from the University of Pisa, and colleagues from the Italian Society of Medical and Interventional Radiology (SIRM).
"The structured report is conceived as a guideline, to recommend the key items/findings of chest CT in COVID-19 pneumonia," they explained in an open-access article published online by Insights into Imaging on 12 August.