Over 3,000 registrants accessed the recent ESR Connect webinar on the clinical presentation of COVID-19 respiratory failure. Dr. Nicola Sverzellati, a thoracic radiologist and head of the radiology unit at the academic hospital of Parma, presented guidance on how radiologists across the world can deal with the crisis.
A frequently asked question is: Can you differentiate COVID-19 from other viral pneumonia? Sverzellati said the literature shows CT findings are entirely nonspecific and depict the most common form of pulmonary response to infections and other disorders: diffuse alveolar damage and organized pneumonia. He noted that in COVID-19, a number of nonspecific findings have been described, such as the crazy-paving, halo, and reverse atoll signs. However, there are other visible clues.
"Pay attention to the shape of abnormality. It's rounded, and this is more unusual compared to other types of infection and is not frequently seen in other disorders," he told viewers, adding that some atypical findings can help with differential diagnosis but that further investigation was needed to define typical signs and patterns.
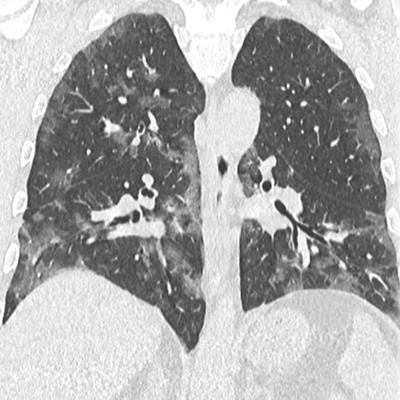
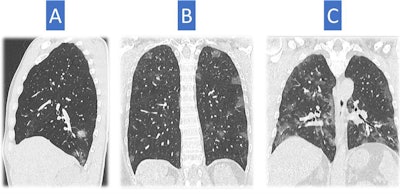 CT scans of three different patients depict typical findings for COVID-19 pneumonia. These look different in severity. Image A shows patchy rounded ground-glass opacities, essentially distributed in the right lower lobe. This is not an unusual feature of infection; therefore, it is difficult to make a differential diagnosis with x-ray. Image B shows several ground-glass opacities, rounded in shape and distributed mainly in the superior regions of the lung, a classic distribution of COVID-19 pneumonia-related abnormalities. Image C depicts ground-glass opacities that are more severe in extent with patchy distribution, occupying a greater volume of the lung. All findings are typical of COVID-19 pneumonia but are not very specific. All images courtesy of Dr. Nicola Sverzellati.
CT scans of three different patients depict typical findings for COVID-19 pneumonia. These look different in severity. Image A shows patchy rounded ground-glass opacities, essentially distributed in the right lower lobe. This is not an unusual feature of infection; therefore, it is difficult to make a differential diagnosis with x-ray. Image B shows several ground-glass opacities, rounded in shape and distributed mainly in the superior regions of the lung, a classic distribution of COVID-19 pneumonia-related abnormalities. Image C depicts ground-glass opacities that are more severe in extent with patchy distribution, occupying a greater volume of the lung. All findings are typical of COVID-19 pneumonia but are not very specific. All images courtesy of Dr. Nicola Sverzellati.Moderator Dr. Adrian Brady from Mercy University Hospital in Cork, Ireland, posed further questions from European Society of Radiology (ESR) members pertaining to the role of plain chest x-ray and other modalities, suggesting it might be reasonable to consider that if CT is available, there may be little or no role for x-ray diagnosis.
CT should be the mainstay of imaging, Sverzellati noted. Chest x-ray has several limitations, and the American College of Radiology has underlined that x-ray proved to be useless in acute pneumonia in previous studies. However, CT should not be considered a screening tool, he added. Although there are mixed opinions on the topic, he believes that CT should be considered in patients with symptoms.
"Triage clinical findings, and then consider CT especially when differential diagnosis with other disorders is not clear and when comorbidities are present or suspected, notably heart failure, which is a very good mimicker, and other chronic disorders," he said.
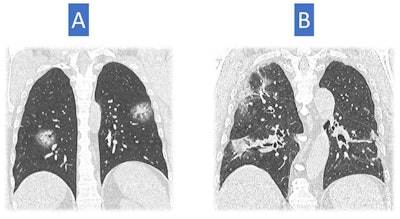 Image A shows larger opacities rounded in shape and some consolidation with a halo of ground glass. This sign has been described in COVID-19 cases. Consolidation is also present in image B, but the consolidation looks a bit different with architectural distortion, consistent with an organizing phase of COVID-19 pneumonia. These show a later stage of pneumonia than in the first three examples.
Image A shows larger opacities rounded in shape and some consolidation with a halo of ground glass. This sign has been described in COVID-19 cases. Consolidation is also present in image B, but the consolidation looks a bit different with architectural distortion, consistent with an organizing phase of COVID-19 pneumonia. These show a later stage of pneumonia than in the first three examples.He noted that CT scans may be helpful for very specific indications but stressed that it was risky to provide a single strict diagnostic flowchart. Patient diagnosis depends on the endemic environment, namely the pretest probability, and the internal resources of the hospital.
"If you have two dedicated CT scanners ... you could consider CT for a broader group of subjects with specific indications," he said, reiterating that CT should not be used as a screening tool. If CT is unavailable, hospitals could use chest x-ray combined with ultrasound and other diagnostic tools.
Key findings from Parma
In the first two weeks of the pandemic (29 February to 13 March), the majority of the 806 CT scans performed showed typical positive findings (549 patients, or 68%) and a sizeable proportion had negative CT results, i.e., normal or highly suggestive of an alternative diagnosis (179, or 22%). A total of 78 scans (10%) were indeterminate.
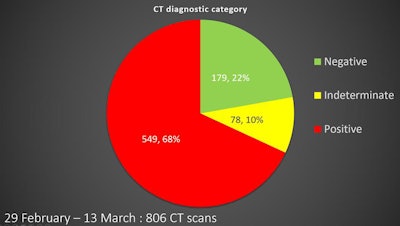 The pie chart shows the percentage of positive, negative, and indeterminate CT scans in Parma between 29 February and 13 March.
The pie chart shows the percentage of positive, negative, and indeterminate CT scans in Parma between 29 February and 13 March.With time, there was a shift in the proportion of positive and negative scans: There was a sizeable proportion of negative and indeterminate CT scans in the first week of March, but the proportion of positive cases and severe disease at CT increased drastically in prevalence toward the middle of the month.
"CT at the beginning was very valuable for differential diagnoses and helping clinicians interpret the clinical findings. But in the new endemic environment, the likelihood of seeing classic COVID-19 pneumonia is high," he said, pointing to a trend of increasing chest x-ray for classical clinical presentation of COVID-19 pneumonia.
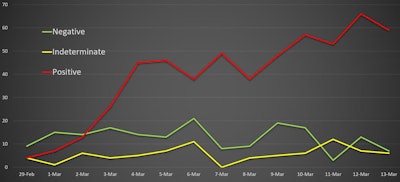 The graph shows change over time in the ratio of positive, negative, and indeterminate CT scans between 29 February and 13 March.
The graph shows change over time in the ratio of positive, negative, and indeterminate CT scans between 29 February and 13 March.Brady was keen to know how Parma had freed hospital capacity and segregated patients.
Sverzellati noted that Parma was not fully prepared for the crisis, but he pointed to a dynamic solution that involves beds increasing in number on a daily basis and the hiring of more staff. Now, over half the 550 internal medicine beds and 60 intensive care unit (ICU) beds are dedicated to COVID-19 patients, and these are in two opposite wings, removed from the emergency department.
Ultrasound assessment
Is there a case for ultrasound assessment and follow-up?
According to Sverzellati, the answer isn't straightforward. While ultrasound is reported as being used in critically ill patients by intensivists, it should be viewed as a complement rather than a substitute, and one that is highly operator-dependent. Radiologists shouldn't give up on x-ray and CT for a reliable description of lung parenchyma. Ultrasound results show some correlation with clinical course, but further confirmation is needed to understand if chest ultrasound can be used instead of other clinical methods for specific questions, he noted.
For CT, one registrant wanted to know if 2.5 mm or thicker slices were sufficient for diagnosing COVID-19. The answer was a resounding no: Ground-glass opacities can be very small and focal, so resolution needs to be optimal for spotting these abnormalities. A 1-mm thick slice is optimal for scanning patients with suspected COVID-19 pneumonia.
 Dr. Nicola Sverzellati is head of radiology at the academic hospital of Parma.
Dr. Nicola Sverzellati is head of radiology at the academic hospital of Parma.Sverzellati also noted that CT gantry cleaning in Parma is down to around 20 minutes between each patient. At the beginning of the pandemic, there wasn't enough staff to conduct a deep clean around the clock, but now the gantry is cleaned after each scan with a full deep clean every 12 hours. This seems to be the best way not to slow down the workflow, he said.
Another ESR member asked if, in Parma, radiologists were routinely extending abdominal CT scans to include the chest. In fact, very few abdominal scans are being performed in Parma and only on patients who have undergone surgery. These patients are not undergoing additional chest CT, Sverzellati clarified. He also shed light on how to manage the risk of complications.
"COVID-19 pneumonia patients will be prone to embolism and thrombosis in the legs, so I sporadically scan patients [with contrast] for suspected pulmonary embolism," he explained. "We haven't found any in our patients so far."
Sverzellati said it is difficult to identify peripheral pulmonary embolism with the presence of widespread ground-glass opacification and motion artifacts, and it is similarly difficult to evaluate pulmonary perfusion in the peripheral regions of the lung.
And have there been any seriously sick children? Out of 30 pediatric x-rays, 20 were confirmed as COVID-19 pneumonia, and the remaining 10 were still under investigation at the time of the webinar. The chest x-rays did not show severe disease, and the children were not very ill, mirroring reports in the literature.
The situation will further change over the coming days and weeks, he continued. Last week, Italy's death toll had already overtaken the toll in China, and the country is now in lockdown, most likely beyond the official limit of 3 April. It is too soon to say whether there is a light at the end of the tunnel, he concluded.
The webinar video is available on demand on the ESR website and on YouTube. This is the most successful ESR Connect Weekly episode in terms of registrations and live viewers so far, according to an ESR spokesman.