The evolution of atrophy rating scales and structured reporting is contributing to MRI's rapidly developing role in a dementia clinical setting, but training and education and implementation challenges remain, according to award-winning Spanish research presented at RSNA 2019 in Chicago.
"Brain imaging is recommended in all current diagnostic dementia guidelines. Recently, they also recommend the application of atrophy rating scales to assess structural changes in the brain of elderly patients, such as medial temporal lobe atrophy by Scheltens," noted Dr. Marta Calvo-Imirizaldu and colleagues from the radiology department of the University Clinic of Navarra in Pamplona, Spain.
"However, there is still low uptake in a routine clinical setting, and knowledge of the neuroimaging strategies available and MRI rating scales is needed in order to encourage clinicians and radiologists to use them," they explained in a digital poster that received a certificate of merit from RSNA judges.
Knowledge gaps
The group sought to identify the most important neuroimaging findings in normal brain aging, to determine the importance of structured reporting in a dementia clinical setting, and to elaborate on the use of MRI in the evaluation of cognitive impairment or dementia, particularly the role of different proposed and established rating scales for specific brain regions.
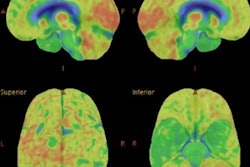
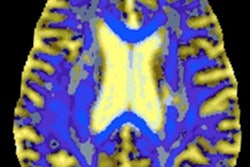
The most relevant structural radiological findings identified from CT and/or MRI in cerebral aging include cerebral/hippocampal atrophy, ventriculomegaly, cerebrovascular disorders, and the presence of microbleeds, the researchers stated. These findings are identified in both normal and pathological aging. Typically, age-related changes are characterized by being less rapid and generally less severe than those of neurodegenerative diseases.
Questions that need to be addressed include the following: Is normal aging a cause or a precursor to neurodegenerative diseases? To what extent do these aging alterations affect brain function? Is pathological degeneration an expression of accelerated aging?
The key neuroimaging techniques in cognitive impairment and dementia are MRI, CT, and FDG-PET. The MRI protocols are laid out below.
| Neuroimaging techniques in cognitive impairment and dementia | ||
| MRI protocol in dementia | Utility | |
| Sagittal T1-weighted (sag T1w) | 3D magnetization prepared rapid gradient echo (MPRAGE) isotropic voxels + coronal reformat perpendicular to hippocampi | Assessment of patterns of atrophy, including medial temporal lobe and hippocampal atrophy. Potential to perform MR volumetry. |
| Transverse fluid-attenuated inversion-recovery (tra FLAIR) | 3-mm slices, 1-mm isotropic voxels | To assess global cortical atrophy (GCA), vascular white-matter hyperintensities, and infarctions. |
| Transverse T2-weighted (tra T2w) | 3-mm slices, 1-mm isotropic voxels | To assess infarctions, in particular lacunar infarctions in the thalamus and basal ganglia, which can be missed on FLAIR images. |
| Tra T2w* or susceptibility-weighted imaging (SWI) | Gradient echo, 3-mm slices, echo time (TE) > 20 msec, small flip angle | To detect microbleeds in amyloid angiopathy. These images can also depict calcifications and iron deposition. |
| Diffusion-weighted imaging (DWI) | Should be considered as a supplemental sequence | Especially in young patients or in rapidly progressive neurodegenerative disorders (degenerative disk disease - vasculitis, Creutzfeldt-Jakob disease). |
If there are contraindications for MRI, multidetector CT will enable coronally reformatted images to be reconstructed perpendicular to the long axis of the temporal lobe for optimal visualization of the hippocampus, the authors continued. FDG-PET is a secondary modality that can be used if the clinical presentation is difficult or unusual, if MRI is inconclusive, and when a molecular diagnosis is required (e.g., assessment of amyloid status).
The role of MRI in suspected cases of dementia is to exclude treatable causes and assess brain atrophy in order to evaluate normal brain aging, identify specific atrophy patterns of neurodegenerative diseases, differentiate cases from other dementias, and identify imaging biomarkers that can help provide an early diagnosis and/or predict conversion, they added.
MRI findings in different entities presenting with dementia are as follows:
- Alzheimer's disease: medial temporal lobe atrophy (MTA) and parietal atrophy
- Dementia with Lewy bodies: no specific MRI abnormalities, in contrast to other forms of dementia
- Frontotemporal lobar degeneration: asymmetric frontal lobe atrophy and temporal-pole atrophy
- Vascular dementia: lobal atrophy, diffuse white-matter lesions, lacunes, and so-called strategic infarctions
When studying MR images, it is essential to systematically score for global atrophy, focal atrophy, and vascular disease (as infarcts, white-matter lesions, or lacunes), the authors wrote. This standardized assessment of the MR findings in a patient suspected of having a cognitive disorder includes the global cortical atrophy (GCA) scale, the MTA scale (Scheltens, 1991), parietal atrophy (Koedam, 2011), the Fazekas scale for white-matter lesions, and looking for so-called strategic infarcts.
Normal aging brain
In a normal aging brain, brain atrophy is hypointense on T2* or susceptibility-weighted images and differential with calcium ions (Ca2+) or deoxygenated blood in veins, they pointed out. Cerebral microbleeds are characterized by mild and symmetric ventricular enlargement with proportionate prominence of the subarachnoid spaces (hydrocephalus ex vacuo) and thinning of the grey matter and decreased white-matter volume, and volumetry by image analysis algorithms for tissue and structure quantification aids in distinguishing normal from abnormal atrophy.
Enlarged perivascular spaces are located in the inferior basal ganglia, centrum semiovale, mesencephalon, and subinsular region, whereas intracranial arterial Ca2+ is present in the intracranial part of the internal carotid artery (i.e., carotid siphon).
White-matter hyperintensities are visible on T2-weighted and fluid-attenuated inversion-recovery (FLAIR) images and are hypodense on CT. There are few, scattered nonconfluent or diffuse areas, bilateral, and the locations are the periventricular and centrum semiovale/subcortical white matter. There is a thin, periventricular hyperintense rim around lateral ventricles or frontal horns.
Silent brain infarctions comprise lacunes, cortical microinfarcts, and small cerebellar infarcts. They are "silent" by definition, being without clinical symptoms or subtle cognitive deficit.
On the other hand, iron deposition is hypointense on T2* or susceptibility-weighted imaging. The locations are globus pallidus, pars reticulata of substantia nigra, dentate nucleus, and putamen. The caudate and thalamus are rarely affected, according to the group.