France's breast cancer screening strategy is at a crossroads, with urgent decisions pending about the use of digital breast tomosynthesis (DBT) and digital second reading of exams. Recent deviation from European norms in quality control, however, could affect patient safety, according to leading educator Dr. Luc Ceugnart.
 Dr. Luc Ceugnart.
Dr. Luc Ceugnart.The design of French breast cancer screening places it beyond most European and U.S. models, and France enjoys a higher than average rate of cancer detection, with 6.7 cancers per 1,000 screens, compared with an average of 5.5 per 1,000 across European countries. Worldwide, the jury is out on France's approach to screening, while the country's imaging community remains unrepentant about its methods.
The strength of the national screening program lies in the fact that it is decentralized, meaning it can take place locally -- in any of the 2,700 centers across France that provide mammography -- and can be tailored to the patient, according to Ceugnart, who is head of imaging at the Oscar Lambret Centre in Lille. Ultrasound is offered systematically to patients with dense breasts, and it is performed at the same screening consultation by a radiologist, rather than in a follow-up appointment.
In the case of anomalies, radiologists may perform a diagnostic DBT exam, which, so far, is not authorized for systematic screening purposes in the healthy population due to further irradiation on top of the amount received from standard mammography.
Quality control
However, a controversial decision from the country's national agency for medical safety (ANSM) to water down quality control on DBT has been met with criticism from the imaging community.
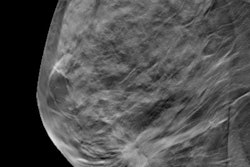
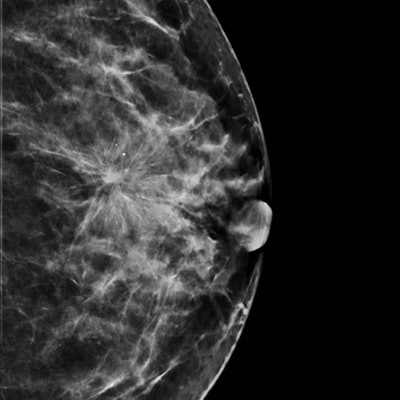
 Synthetic image reconstructed from DBT data. All images courtesy of Dr. Luc Ceugnart.
Synthetic image reconstructed from DBT data. All images courtesy of Dr. Luc Ceugnart.Rather than using the entire European Reference Organisation for Quality Assured Breast Screening and Diagnostic Services (EUREF) protocol for DBT, French quality control will implement an identical protocol for dose measurement, but without image quality control protocols in place, according to Ceugnart.
The risk is that some vendors will use lower doses to be validated, without any checks on image quality, when the correct dose is crucial for accurate cancer detection, he noted. This lower level of control is insufficient and could be damaging to vendors, radiologists, and women being examined, he added.
"We would have preferred to keep the European version of stricter quality control on DBT, rather than the 'light' version, which may prove detrimental to patients," Ceugnart told AuntMinnieEurope.com.
DBT is validated for diagnosis in the case of abnormal findings, as it is in most European countries. However, France's high health authority (Haute Autorité de Santé, or HAS) this year is due to publish an official guideline on using DBT for screening, following the receipt of a literature review on the modality's performance.
Presenting an outline of the review at the recent national congress, JFR 2019, Ceugnart noted that combining mammography and DBT seemed to yield better detection rates than mammography alone. However, complementary studies are needed to obtain more robust results, particularly in terms of interval cancer rates. He also pointed to the possibility of synthesized images generated from DBT datasets to avoid additional radiation exposure.
Tailored screening
The current approach to screening has worked well in France, according to Ceugnart, who moderated the breast cancer screening session "We're going forward -- but to where?" at JFR. The consensus among the nation's experts is that there has been no real advance in the past 12 months, but that in some respects France's screening program is already ahead.
While other societies may have expressed doubt over French methods as being "too much" -- and too expensive, the country's imaging community seems at peace with its stance on complementary ultrasound, which has been supported by studies from abroad in recent years.
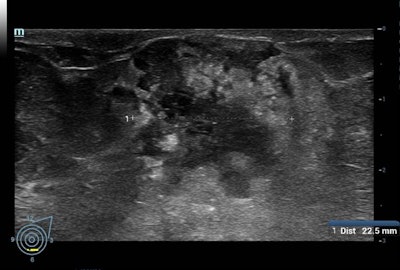 Above: A BI-RADS 5 mass visualized on ultrasound. Below: The same mass, vascularized in doppler.
Above: A BI-RADS 5 mass visualized on ultrasound. Below: The same mass, vascularized in doppler.For example, the Adjunct Screening With Tomosynthesis or Ultrasound in Women With Mammography-Negative Dense Breasts (ASTOUND) study showed that ultrasound has better incremental breast cancer detection than DBT in mammography-negative dense breasts at a similar false-positive recall rate. However, DBT detected more than 50% of the additional breast cancers in these women, according to the authors.
Meanwhile, the Japan Strategic Anticancer Randomized Trial (J-START) revealed that adjunct ultrasound increased sensitivity and the detection rate of early-stage cancers.
"We've been performing complementary ultrasound for 20 years, so in this respect we are ahead of the game. It might be more expensive, but it is more effective and definitely more human," he told AuntMinnieEurope.com. "This may be the juncture at which other countries start following suit for screening."
Still, there are issues that need resolution, according to Ceugnart.
Digitalization for second reading in screening programs is also under scrutiny, and French radiologists are eagerly awaiting the results of a study on the accuracy and feasibility of digital second reads. The national cancer institute (INCa) has been trialing the strategy at four sites in France over the past three years, but no results have been published.
Without concrete results due to delays in the experiment, second reads need to continue on film, Ceugnart noted, which will slow the screening effort in the short- to midterm, particularly in terms of digital imaging's cost-effectiveness.