With greater use of high-resolution cross-sectional imaging, many more renal masses are detected in routine practice. But how can doctors determine the best therapeutic approach to improve patient outcomes?
Accurate and early characterization of these pathologies through multiparametric MRI (mpMRI) could soon become pivotal in patient management. New protocols are now gaining ground but large-scale clinical validation is ongoing.
Speaking during the Renal Tumors for Idiots session at the recent French national congress (JFR) in Paris, Dr. Nicolas Grenier from Centre Hospitalier Universitaire Bordeaux described how a newly established protocol being used in a multisite study in France will provide specialists with decisive and timely information.
 Dr. Nicolas Grenier from Bordeaux, France.
Dr. Nicolas Grenier from Bordeaux, France."MpMRI has the potential to characterize these so-called 'indeterminate' solid, renal tumors on CT -- tumors without macroscopic fat or obvious features of malignancy. Papillary carcinomas and fat-poor angiomyolipomas will probably the easiest to recognize, but we need more experience to confirm this and to identify the other subtypes," Grenier told AuntMinnieEurope.com during the congress. "This could have an impact on patient management in the future, in terms of deciding on surgical or percutaneous management or on active surveillance, without biopsy. The impact on practice will be higher for urologists than for oncologists who are dealing with more advanced malignant tumors."
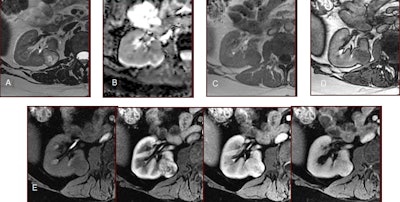
Following two promising single-center studies, the Bordeaux study IRMK01, which focuses on mpMRI's capacity for tumor differentiation, began in the last quarter of 2018 and will run for two years. It forms part of the French Ministry of Health's project for clinical research in hospitals (Projet Hospitalier de Recherche Clinique), which funds a number of national clinical trials.
Set to involve 500 patients across 16 centers, the aim of IRMK01 is to evaluate the accuracy of mpMRI by scoring a specific protocol on a five-point Lickert scale for classifying tumors that were indeterminate on CT as benign or malignant. As a secondary focus, the study will evaluate mpMRI's effect on management decisions.
Different sequences available on MRI have allowed huge growth in criteria used for defining characteristics that are specific to different tumor types, and this can be particularly helpful for small, solid tumors smaller than 4 cm that are indeterminate in CT, noted Grenier, a professor of radiology and the head of urogenital and vascular radiology at hospital Pellegrin in Bordeaux.
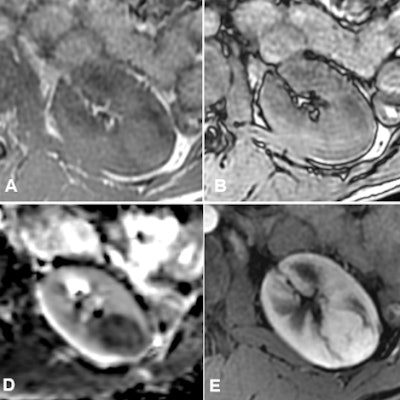
 Typical appearance of a fat-poor angiomyolipoma: isointense or very slightly hyperintense in T1 (A), with or without a signal drop on opposed-phase image (B), hypointense in T2 (C), with clear diffusion restriction on the apparent diffusion coefficient (ADC) map (D), hyperarterialized and with a rapid washout (F). Image courtesy of Dr. Nicolas Grenier, and Société française de radiologie (SFR) -- reproduced with permission from the SFR's e-Quotidien des JFR.
Typical appearance of a fat-poor angiomyolipoma: isointense or very slightly hyperintense in T1 (A), with or without a signal drop on opposed-phase image (B), hypointense in T2 (C), with clear diffusion restriction on the apparent diffusion coefficient (ADC) map (D), hyperarterialized and with a rapid washout (F). Image courtesy of Dr. Nicolas Grenier, and Société française de radiologie (SFR) -- reproduced with permission from the SFR's e-Quotidien des JFR.The new mpMRI protocol in play at Bordeaux for differentiation is now being validated for diagnostic accuracy. In the protocol, the most useful sequences for characterization are as follows:
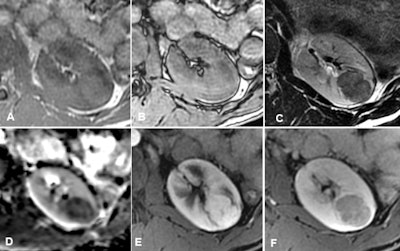
- T2-weighted sequences: These must be performed strictly with turbo or fast spin echo and never in T2-weighted fast gradient echo. This allows the evaluation of the tumor's signal strength compared with the kidney. Only fat-poor angiomyolipoma (fpAML) and type 1 papillary carcinoma have a much lower signal than the kidney.
- T1-weighted gradient-echo sequences with chemical shift (Dixon) imaging: A drop in signal can be seen in opposed-phase in cases of fpAML, clear cell carcinoma, or papillary carcinoma and in in-phase images in cases of papillary carcinoma.
- Diffusion sequences: With these also, only cases of fpAML and papillary carcinoma have a much lower signal than the kidney.
- Dynamic sequences after injection of contrast media allow the "plotting" of enhancement: Only cases of papillary carcinoma show very poor and very progressive enhancement.
Through comparing and combining these different criteria, radiologists can arrive at different, more specific diagnoses, Grenier noted.
The most commonly seen benign kidney tumors are fat-poor angiomyolipomas -- without any fatty tissue visible on CT without injection -- and oncocytomas. The most frequent malignant tumors are clear cell carcinomas, type 1 papillary carcinoma, and chromophobe carcinoma.
 Typical aspect of a clear cell carcinoma showing, compared with normal renal parenchyma, a high signal intensity on T2 (A), a high ADC (B), a drop of signal on opposed-phase image (D), compared with the in-phase (C), and a high vascularity on the dynamic contrast-enhanced image (E). Image courtesy of Dr. Nicolas Grenier.
Typical aspect of a clear cell carcinoma showing, compared with normal renal parenchyma, a high signal intensity on T2 (A), a high ADC (B), a drop of signal on opposed-phase image (D), compared with the in-phase (C), and a high vascularity on the dynamic contrast-enhanced image (E). Image courtesy of Dr. Nicolas Grenier.Specifically, the researchers hope to use the data from the large prospective study to evaluate mpMRI for differentiating small, solid, malignant, renal tumors from benign tumors and also to check the reproducibility and effect on clinical decisions and tumor management, as well as define the criteria that allow lesion classification.
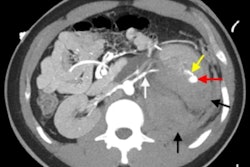
For a long time, CT characterization of kidney tumors was divided into classifying cystic masses using the Bosniak classification method and identifying macroscopic fatty elements allowing the diagnosis of angiomyolipoma, while diagnosis of carcinoma was based on tumors with a necrotic aspect or signs of local extension, according to Grenier.
Today, however, incidental findings of little solid masses during imaging are the main mode of diagnosing kidney cancer. Among these masses, the proportion of benign tumors is all the more important because they are small, he stated.
"Gradually, MRI has gained ground for Bosniak classification in difficult cases. However, its place in solid tumor differentiation is only just emerging," Grenier said.