Researchers from France have used augmented reality technology to overlay 3D models based on MRI scans onto a real-time video of the uterus, helping clinical staff to locate tumors and determine the best approach for their surgical removal. The results were recently published online in the Journal of Minimally Invasive Gynecology.
Adenomyomas, or inner uterine tumors, occasionally lead to excessive uterine pain or abnormal bleeding and require laparoscopic surgery. The challenge with this procedure is that adenomyomas are very soft and often positioned deep within the uterine muscle, limiting the amount of information that clinicians are able to draw from standard endoscopic imaging and tactile feedback, noted first author Dr. Nicolas Bourdel, PhD, and colleagues from Université Clermont Auvergne.
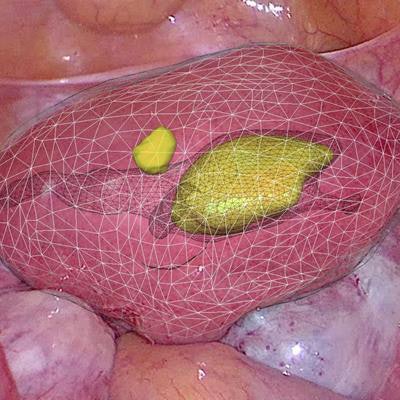
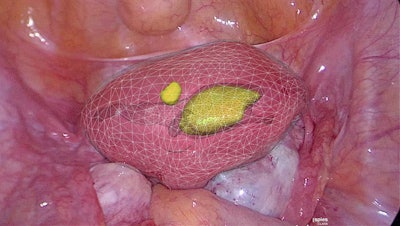 Augmented reality displaying a 3D model of an adenomyoma overlaid on top of the patient anatomy. Image courtesy of Dr. Nicolas Bourdel, PhD.
Augmented reality displaying a 3D model of an adenomyoma overlaid on top of the patient anatomy. Image courtesy of Dr. Nicolas Bourdel, PhD.In contrast to conventional imaging viewed on 2D screens, augmented reality (AR) provides clinicians with a complete 3D view of subsurface anatomical structures and tumors, and it also allows "information from preoperative imaging, such as MRI, to be overlaid and fused in real time with endoscopic imagery," they wrote.
In the current case study, Bourdel and colleagues developed an AR technique that allowed clinicians to visualize 3D models of the uterine cavity and tumors while performing laparoscopy on two patients with adenomyomas (J Minim Invasive Gynecol, 6 April 2019).
The researchers generated the models by obtaining the patients' MRI scans, segmenting the tumors and surrounding anatomy from the scans using segmentation software, and converting the images into AR 3D models. During laparoscopy, gynecologic surgeons were able to see these AR 3D models on a screen that displayed a real-time video of the patient, as well as overlay the models onto their corresponding location on the screen.
Although segmenting the MRI scans was time-consuming, the actual construction of the AR 3D models and registering the images onto the actual anatomy took less than five minutes. Ultimately, the AR technique enabled the operating surgeon to locate the adenomyomas in both patients as well as establish the ideal entry point and depth of the incision before removing the tumors.
The technique also allowed the surgical team to complete both laparoscopies with increased accuracy, according to the researchers. In the future, clinicians may be able to use AR 3D models to improve presurgical planning and pathology localization for a wide range of procedures.
"The [AR] software takes into account the mobility of the uterus and thus differs markedly from nongynecological uses of AR, opening the way to making laparoscopic adenomyomectomy easier, safer, and faster," they wrote. "With just small modifications this technique may be used for the majority of gynecological surgeries and so facilitate the localization of anatomic markers."


















