The ability to assess the impact of radiation on malignant tumors during a course of radiotherapy could help improve its effectiveness for individual patients. Based on tumor response, physicians could modify the treatment regimen, dose, and radiation field accordingly.
Israeli researchers have now demonstrated that thermography may provide a viable radiotherapy monitoring tool for such treatment optimization. They have developed a method to detect tumors in a thermal image and estimate changes in tumor and vasculature during radiotherapy, validating this in a study of six patients with advanced breast cancer (Journal of Biomedical Optics, May 2018, Vol. 23:5, pp. 1-6).
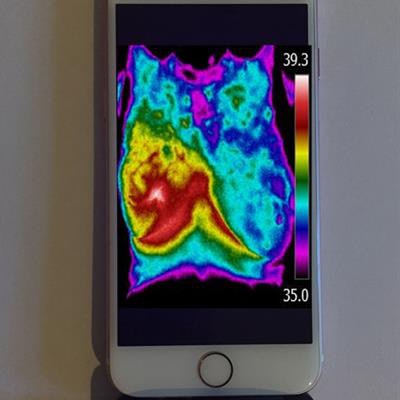
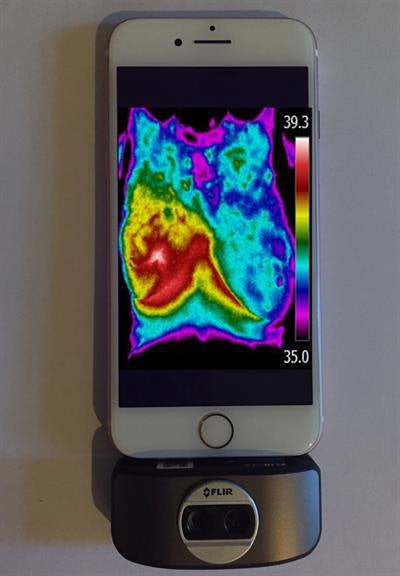 Thermal images recorded on a smartphone with thermal camera attachments. Image courtesy of Israel Gannot.
Thermal images recorded on a smartphone with thermal camera attachments. Image courtesy of Israel Gannot.Thermography had been rejected as a breast cancer detection tool due to its suboptimal sensitivity and specificity. However, for an already detected tumor undergoing radiation or chemotherapy, it could prove a highly effective monitoring tool when incorporating algorithms developed by the research team.
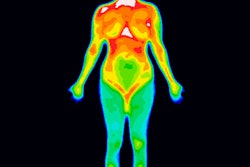
The multi-institutional team had conducted research on thermal imaging to understand tumor aggressiveness in animal models. They hypothesized that because malignant tumors are characterized by abnormal metabolic and perfusion rates, they will generate a different temperature distribution pattern compared with healthy tissue. By measuring skin temperature maps at the tumor location before and during treatment, the reaction of a tumor to radiotherapy can be measured.
Israel Gannot, PhD, professor of biomedical engineering at Tel-Aviv University, and co-authors, developed a four-step algorithm to analyze the thermal images. First, images were converted from color to gray scale and a fixed temperature range of 7°C set for all images, to enable comparison of the entropy (which characterizes the homogeneity of the image) in different images. Images were filtered using a Frangi filter designed to emphasize tubular structures. This filter highlighted blobs of heat (the malignant tumor) and long, narrow, tubular objects (the blood vessel network). Images were enlarged sevenfold to observe local temperature changes in the blood vessels.
In the final step, feature extraction, the algorithm calculates entropy in the cropped thermal image of the tumor area and in the filtered tumor image. It then estimates changes in tumor regularity and vasculature shape during radiotherapy.
Patient imaging
The six patients were women with stage IV breast cancer and distant metastatic disease. None had undergone surgical resection of their tumors, which had a diameter larger than 1 cm at a depth of less than 1 cm. All patients received 15 radiation fractions of 3 Gy, administered over three weeks.
 Researchers (left to right) Israel Gannot, professor of engineering in the Department of Biomedical Engineering at Tel-Aviv University, Merav Ben-David, head of the Radiation Oncology Department of Sheba Medical Center, and doctoral student Oshrit Hoffer.
Researchers (left to right) Israel Gannot, professor of engineering in the Department of Biomedical Engineering at Tel-Aviv University, Merav Ben-David, head of the Radiation Oncology Department of Sheba Medical Center, and doctoral student Oshrit Hoffer.The patients underwent thermal imaging before each radiotherapy session and a day after the end of the session. Room temperature and humidity were controlled during image acquisition and fluorescent lights were turned off. The thermal camera, positioned 1 m from the patient, acquired images containing either 320 x 256 or 320 x 240 pixels.
The authors report that entropy was reduced in the tumor areas, for all patients, during radiation treatment. They described the appearance of the tumor vasculature as "a crab with many arms." To quantify changes in the shape of vascular networks, they converted the images into binary images and counted the number of objects before and after radiotherapy. They saw a reduction in the number of objects, indicating a reduction in the vessels supplying nutrients to the tumor.
Expanding applications
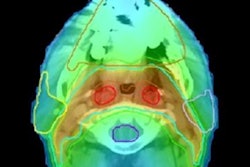
The researchers selected breast cancer for the initial research because co-researcher Dr. Merav Ben-David, clinical fellow at Sheba Medical Center, specializes in breast cancer treatment. They are now looking at additional applications, such as the treatment of cervical cancer and head-and-neck cancer.
"We are collecting more data to run big data statistics," Gannot tells Physics World. "We are also starting to implement the use of this technology as a tool for early warning of breast cancer by women at their home, using a thermal camera attached to a cell phone with our algorithms implemented in the smartphone app. This is intended for use in addition to mammography. It could fill the time span between mammography examinations when many cancers develop."
In future research, the authors are planning to use thermal imaging devices with multiple angles and perform real-time analysis. They are planning larger studies to evaluate the efficacy of thermography to monitor radiotherapy, chemotherapy, and immunotherapy treatments.
© IOP Publishing Limited. Republished with permission from Physics World, a website that helps scientists working in academic and industrial research stay up to date with the latest breakthroughs in physics and interdisciplinary science.