A follow-up study by German researchers has pinpointed the presence of frontotemporal lobar degeneration (FTLD) as the determining factor to explain why Alzheimer's patients with amyloid-positive PET scans can outlive patients with negative amyloid results.
The research, presented at the 2018 annual meeting of the Society of Nuclear Medicine and Molecular Imaging (SNMMI), also reinforced evidence that patients with FTLD are considerably more likely to have shorter survival times than Alzheimer's patients.
"With a combination of Pittsburgh Compound B (PiB)-PET and FDG-PET, we could link the higher mortality rate of those amyloid-negative patients to the FTLD, which lines up with known studies," said lead presenter Johannes Fostitsch, from the Clinic for Nuclear Medicine at the University of Freiburg. "That also explains why we had a relatively longer survival for the amyloid-positive patients with suspected dementia."
Shorter survival
Past research has shown that patients with dementia generally have a shortened life span. Naturally, confirmation of a dementia diagnosis can have a devastating effect on these patients, Fostitsch pointed out.
"They have a lot of questions, most of them regarding the prognosis," he added. "That is why we focused on PiB-PET to find out if there is also a prognostic value, besides its already well-known diagnostic value for patients who are examined as part of their dementia diagnostics."
This most recent study follows similar research, which Fostitsch and colleagues presented at last year's annual SNMMI meeting. Their earlier study examined the prognostic value of amyloid-PET imaging in patients with suspected dementia.
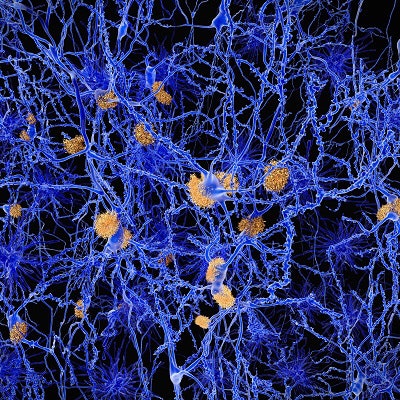
In that study, the researchers rather surprisingly found a better prognosis for patients with amyloid-positive PET scan results likely due to the fact that a significant number of amyloid-negative patients have a form of dementia associated with FTLD. In those cases, people with FTLD have a worse prognosis than patients with Alzheimer's, according to Fostitsch and colleagues (Journal of Nuclear Medicine, May 1, 2017, Vol. 58:suppl 1255).
The patients with an amyloid-negative PET result and FTLD had a 2.8-times greater risk of dying than amyloid-positive patients with no FTLD. Interestingly, the overall median time of survival for amyloid-negative patients was 6.5 years, which was not reached by amyloid-positive patients, according to the 2017 study.
"From there, we had two goals: to confirm amyloid as a predictor using a longer follow-up period, and to elucidate our findings using a combination of the PiB-PET and FDG-PET," Fostitsch told SNMMI 2018 attendees. "In other words, we were trying to see what is behind this finding of a longer survival with amyloid-positive patients."
Prognostic prowess
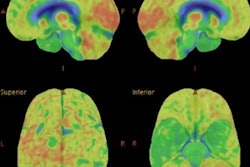
In the follow-up study, the researchers looked at 260 patients from their institution's memory clinic from May 2009 to June 2016. Subjects already were known to have clinical symptoms of cognitive impairment based on previously performed FDG-PET and PiB-PET scans (ECAT, Siemens Healthineers; Gemini TF 64 PET/CT, Philips Healthcare). As a radiopharmaceutical, PiB has been shown to detect amyloid plaque in the brain as a precursor to Alzheimer's disease.
The researchers also were able to confirm survival data on 253 of the patients and the lower mortality risk of amyloid-positive patients, based on the hazard ratio (HR) of 0.5 (range, 0.27-0.9; p < 0.05) in the 2017 study.
"In 166 cases, we also had the Mini-Mental State Examination (MMSE) test scores, which we used as a variable for the progression of dementia in each patient," Fostitsch added.
Of those subjects, 211 patients were divided into three groups based on the combined clinical PiB-PET and FDG-PET results:
- Normal PiB-PET and FDG-PET scans (35 subjects)
- Patients with Alzheimer's disease (121 subjects)
- Patents with FTLD (55 subjects)
Because of such a disparity among the remaining 41 patients, they were distributed across smaller subgroups, given the lack of sufficient numbers for a reliable analysis.
The researchers also lost 37 subjects who died. After a median follow-up time of 4.4 years, 17 people (14%) in the Alzheimer's group died, followed by 15 patients (27%) in the FTLD group (median follow-up of 4.0 years) and five deaths (14%) among subjects with normal scans (median follow-up of 3.8 years).
Mortality risk
An analysis of the three patient groups revealed that patients diagnosed with Alzheimer's by combined PiB-PET and FDG-PET imaging had a significantly lower mortality risk than patients diagnosed with frontotemporal lobar degeneration (HR = 0.4; range 0.21-0.88; p < 0.05). Conversely, patients in the FTLD group also had a shorter life span than subjects in the Alzheimer's group.
The results were confirmed further after excluding all five amyloid-positive patients with FTLD and after adjustments for MMSE dementia progression scores among 166 subjects.
"Once we adjusted for our MMSE scores, we can see that the hazard ratio becomes 2.3, and we have a lower mortality risk for Alzheimer's patients," Fostitsch said. "If we look at the hazard ratio at 2.3, we have twice the mortality risk with the FTLD group, compared to the Alzheimer's group."
When MMSE scores among FTLD patients were added to the calculations, the hazard ratio and risk of mortality increased to 3.2, compared with the Alzheimer's group. The median survival time for the FDL the group was 6.1 years.