Digital breast tomosynthesis (DBT) has the potential to improve healthcare by increasing diagnostic accuracy and simplifying workup in breast cancer assessment clinics, so much so that assessment clinics have widely embraced the modality, a new study published in European Radiology found.
Researchers from Australia randomly allocated breast cancer cases for blinded review of digital mammography workup and DBT workup, in conjunction with a mammogram from the screening examination. They found that 93.3% of radiologists performed better or comparably with DBT than when using standard mammographic workup views, according to first authors Suneeta Mall, a doctoral candidate from the University of Sydney Faculty of Health Sciences, and Dr. Jennie Noakes from Northern Sydney & Central Coast BreastScreen at Royal North Shore Hospital in New South Wales (Eur Radiol, 30 May 2018).
"As a result of this study, DBT has been introduced into all New South Wales BreastScreen assessment clinics and into multiple assessment clinics across Australia," Mall told AuntMinnieEurope.com.
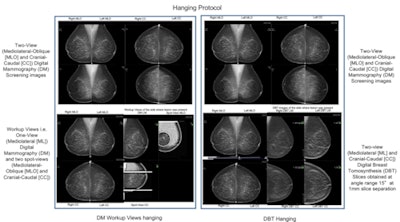
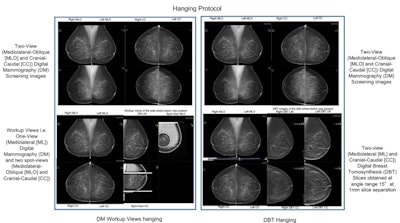
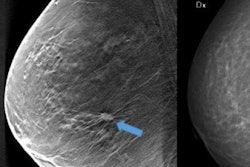
Details of the hanging protocol used for both the digital mammography workup view and DBT assessments. Image courtesy of Suneeta Mall.
She and her colleagues found DBT has the potential for successful use in the assessment clinics in Australia and that DBT, in combination with digital mammography images from the screening examination, provides increased diagnostic accuracy, improves radiologists' performance and confidence, reduces the number of additional images and biopsies required, and even improves patient care by simplifying the assessment workflow.
DBT in the clinic
DBT is being integrated into clinical use as it improves lesion visibility, reduces recall rates, increases cancer detection and diagnostic accuracy, and improves patient comfort. However, most of these results came from breast cancer screening and not assessment clinics.
The aim of the assessment clinic is to confirm the presence of malignancy and refer the patient to treatment, or to reject the screen-detected findings and return the woman to routine screening, according to Mall, Noakes, and colleagues.
"The workflow in the assessment clinic is very complex as it not only requires evaluation of various images but may also involve biopsy," they wrote. "Diagnostic accuracy is critical in assessment; therefore, the need for superior lesion visibility and improved lesion characterization is paramount."
Is DBT up to the task? That's what the researchers sought to determine in their Tomosynthesis Assessment Clinic Trial (TACT). Conducted within the Australian National BreastScreen program, they investigated the efficacy of DBT in breast cancer diagnosis and compared it with the standard digital mammography workup. They evaluated whether DBT in combination with digital mammography images from the screening examination would provide increased diagnostic accuracy, improve radiologists' performance, reduce the number of additional images and biopsies required, and improve patient care.
They included 144 women ages 40 and older recalled to the assessment clinic. The 48 cancer cases were randomly allocated for blinded review of digital mammography workup and DBT, both in conjunction with previous mammograms. The study included 15 radiologists of varying experience levels in the Australia BreastScreen Program -- each radiologist read 48 cases (16 cancers) in three nonoverlapping blocks. Diagnostic accuracy was measured by means of sensitivity, specificity, positive predictive value (PPV), and negative predictive values (NPV). The researchers calculated the radiologists' performances using receiver operating characteristic area under the curve (AUC).
Radiologists graded the lesion severity, lesion conspicuity, and confidence in their assessment on five-point scales with 5 being the highest, i.e., severe malignancy.
A few radiologists identified 30 unique additional lesions (six only in DBT and 14 only in digital mammography, 10 in both DBT and digital mammography), but they were reported a total of 51 times in 31 cases: 23 in DBT and 28 in digital mammography. Most radiologists identified at most one additional lesion, and these did not require further assessment. Except for one radiologist, all radiologists (93.3%) performed better or comparably using DBT.
Results are summarized in the table below:
| Comparison of digital mammography vs. DBT in an Australian clinic | ||
| Digital mammography | DBT | |
| Sensitivity | Primary lesion: 91% All lesions: 90% |
Primary lesion: 94% All lesions: 93% |
| Specificity | Primary lesion: 57% All lesions: 56% |
Primary lesion: 77% All lesions: 75% |
| PPV | 49% | 64% |
| NPV | 92% | 96% |
On average, the AUC for DBT was 0.06 higher than for digital mammography (maximum difference 0.13). The AUCs for DBT (primary lesion 0.935, all lesions 0.927) were higher than for digital mammography (0.876, 0.872).
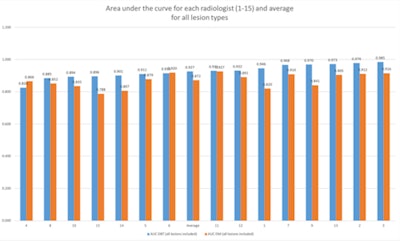
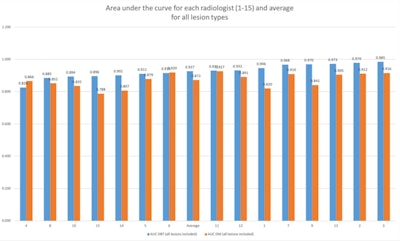
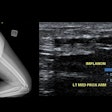
Projection of the radiologists' performance measured by the area under the curve for all lesions (including primary and secondary lesions). Image courtesy of Dr. Suneeta Mall.
In addition, radiologists were more confident about their decisions using DBT, noncancer lesions appeared less severe on the modality, cancerous lesions appeared more severe, and cancerous lesions were more easily seen on DBT. Plus, fewer additional views were required using DBT in both dense and nondense breasts.
Regarding biopsies, DBT led to an overall reduction in biopsy recommendation -- 58.3% for dense breasts for false positives and negatives.
In terms of future research, Mall and colleagues would like to conduct a countrywide assessment that would possibly detect any regional variations in the benefits of use of DBT in the assessment clinic.
"In addition, we used a small number of cases in this study, and carrying out a larger study with more cases would be desirable to improve on the generalizability of the results," she told AuntMinnieEurope.com.