Determining the best occluder device size necessary to properly seal the left atrial appendage (LAA) before implanting the device may be feasible with the assistance of 3D printing, according to two separate presentations at ECR 2018 in Vienna.
Two teams of investigators -- one from Switzerland and the other from Italy -- used different techniques to create individually tailored 3D-printed models of the left atrium of patients who needed to undergo LAA occlusion. By measuring the diameter of the LAA in these models, clinicians were able to preoperatively estimate the appropriate size of the occluder device for most of the patients.
"The key implications of the personalized 3D-printed heart model are that it allows us to simulate the LAA closure procedure, identify the optimal device size and position within the LAA, and reduce the device implantation learning curve," Dr. Anne-Lise Hachulla, a radiologist at Geneva University Hospital in Switzerland, told AuntMinnieEurope.com.
Accurate sizing
In recent years, LAA occlusion has emerged as an alternative therapeutic approach for lowering the risk of stroke in patients who have atrial fibrillation and a contraindication to oral anticoagulation, i.e., warfarin, Hachulla said. Due to the natural variability in LAA structure, one of the major challenges of this technique for clinicians is determining the ideal size of occluding device for LAA closure.
The rise of 3D printing as an aid to surgical simulation and even as a guide for device implantation motivated the Geneva group to evaluate the potential usefulness of 3D printing in facilitating surgeons as they make this decision.
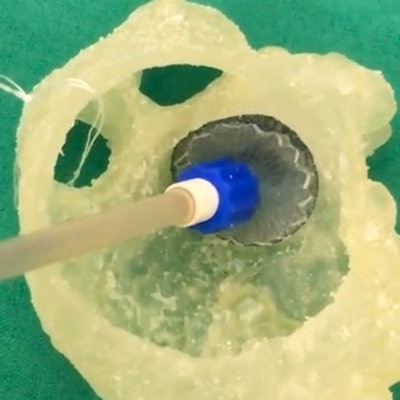
To that end, they measured the mean diameter of the opening to the LAA on the transesophageal echocardiograms and CT scans of 15 patients with atrial fibrillation, and then used the measurements to predict the best size of occluder device for each patient. In addition, they used the CT scans to create 3D models of the left atrium using semiautomatic algorithms in computer software (Vitrea, Vital Images), printed the 3D models out with a 3D printer (Objet260 Connex3, Stratasys), and finally measured the diameters of the LAA.
Segmentation of the CT scans took less than 15 minutes, and 3D printing the left atria took about eight hours. The average price of one of these 3D-printed models was approximately 201 euros.
After the patients underwent percutaneous LAA closure, the researchers recorded the size of the actual implanted occlusion device (Amplatzer Amulet, St. Jude Medical-Abbott) and compared it to the size recommendations from each of the three modalities.
On average, measurements from transesophageal echocardiograms correctly predicted the appropriate size of the occlusion device in 53% of the cases, compared with 67% of cases with those from cardiac CT scans and 100% of the time with those from the 3D-printed models.
"We introduced a fast and robust protocol using a personalized 3D-printed LAA model to select the correct size of the occluding device," Hachulla concluded.
Correct positioning
In a subsequent presentation, Dr. Giuseppe Muscogiuri and colleagues from Centro Cardiologico Monzino in Milan explained how they employed 3D printing to guide their selection of occluder device for LAA closure.
They began by collecting cardiac CT angiography scans of 13 patients affected by atrial fibrillation and then segmenting the scans using the open-source software ITK-Snap. They also smoothed and refined the 3D models before fabricating the patient-specific 3D-printed left atria with a stereolithography printer (Form 2, Formlabs). Finally, two observers measured the diameter of the opening to the LAA in each of these models using a digital caliper.
For the analysis, they compared the estimated sizes of the occluder devices based on measurements of the 3D-printed models to the sizes of the devices actually implanted by surgeons who did not refer to the models.
Out of 13 cases, the suggested size of occluder device from the 3D-printed models either matched exactly or was adequate relative to the actual implant in 12 instances. There was only one case for which the surgically inserted occluder device was larger than the estimated size drawn from the 3D-printed models.
These findings suggest that 3D printing a model of the left atrial appendage can contribute to predicting the correct size of occluder devices and determining its ideal position, as well as providing additional data, Muscogiuri said.
"We think that the left atrial appendage model obtained by 3D printing can help in terms of therapeutic approach in patients with atrial fibrillation," he noted.



















