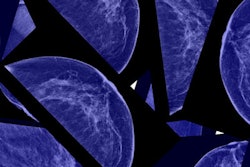
Using digital breast tomosynthesis (DBT) with full-field digital mammography (FFDM) detects more cancers and has improved specificity compared with FFDM alone, according to a large study from Norway by Dr. Per Skaane and colleagues and published in Breast Cancer Research and Treatment.
As part of the Oslo Tomosynthesis Screening Trial (OTST), the researchers compared DBT and FFDM with FFDM alone in breast cancer screening exams from more than 24,000 women. They found screening using FFDM plus DBT demonstrated a cancer detection rate and a higher specificity. Using the two modalities together also resulted in a statistically significant lower recall rate as compared with FFDM-only screening (Breast Cancer Res Treat, 10 February 2018).
"Implementing tomosynthesis in population-based screening significantly improves cancer detection rate, specificity, and number of recalls per screen-detected cancer," wrote the study authors, led by Skaane of the division of radiology and nuclear medicine at the Oslo University Hospital Breast Imaging Center in Oslo. "However, characteristics of the additional FFDM plus DBT-only detected cancers and interval cancers suggest that benefits from tomosynthesis may not be proportional to number of additional cancers and some additional cancers might represent overdiagnosis."
Adding DBT
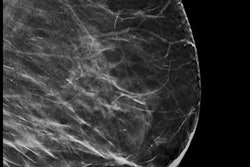
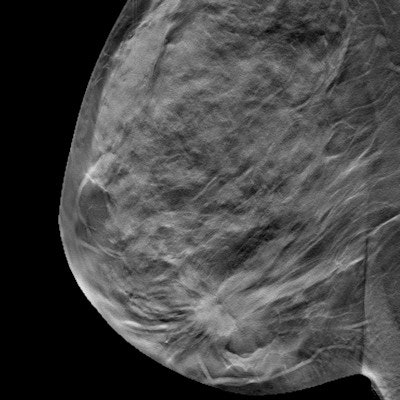
FFDM has been the gold standard of breast cancer screening, but challenges to the modality can include the "masking effect" of overlying parenchyma in dense breasts, while normal parenchyma can sometimes simulate abnormalities. DBT could improve both of those limitations; however, little is known about interval cancer rates following screening with tomosynthesis.
In the new study, Skaane and colleagues reported data at the two-year follow-up point for outcome measures other than mortality in the Oslo Tomosynthesis Screening Trial. The data include sensitivity, specificity, and interval cancer rates from DBT screening as compared with previous FFDM rounds from the screening program.
The screening trial invited women ages 50 to 69 biennially for breast cancer screening. This amounted to 24,301 consenting women undergoing FFDM plus DBT (Dimensions, Hologic) screening over a two-year period. The researchers compared results with 59,877 FFDM (Senographe 2000D, GE Healthcare) exams during prior rounds. The DBT systems automatically determined radiation dose and was set to approximately the same dose as a single mammographic view.
Adding DBT resulted in an increase in sensitivity that was not statistically significant (76.2% versus 80.8%, p = 0.151) and a statistically significant increase in specificity (96.4% versus 97.5%, p < 0.001). Results are summarized in the table below.
| FFDM vs. DBT + FFDM in Oslo Tomosynthesis Screening Trial | ||
| FFDM | FFDM + DBT | |
| Recall rate | 42.3 | 33.7 |
| Screen-detected cancer rate | 6.3 | 9.3 |
| Interval cancer rate | 2.0 | 2.1 |
| Sensitivity | 76.2% | 80.8% |
| Specificity | 96.4% | 97.5% |
| Recalls per screen-detected cancer | 6.7 | 3.6 |
Invasive cancers represented a larger fraction of cancers detected by FFDM and DBT (84.1%,
191/227) compared with previous FFDM rounds (79.9%, 302/378). A smaller fraction of FFDM plus DBT-detected invasive cancers were node-positive (15.6%, 29/186) compared with FFDM detections in previous rounds (21.4%, 64/299).
However, differences in type, grade, and node status were not statistically significant (p ≥ 0.124).
The total number of cancers (screen-detected and interval) during the Oslo Tomosynthesis Screening Trial increased significantly from 8.3 cancers out of 1,000 screens to 11.6 out of 1,000 screens, indicating that adding DBT to FFDM detects additional cancers that may not present as "interval cancers" prior to the subsequent screening round, according to the authors.
The researchers also identified 55 additional FFDM plus DBT-detected ("DBT-only") cancers (three ductal carcinoma in situ and 52 invasive) with three cancers detected by FFDM alone. The "DBT-only" cancers were of lower grade, lower fraction with positive nodes, and smaller in size than the interval cancers.
"The fact that our study did not demonstrate any reduction in interval cancer rate, at least post one round of FFDM plus DBT, and the fact that most of the additionally detected cancers were small node-negative invasive cancers of molecular subtypes known to have a good prognosis raises the question whether the additional DBT-only detected cancer might represent 'overdiagnosis,' " the study authors wrote.
Little is known about tomosynthesis screening and potential overdiagnosis. One study demonstrated sustainable increase in cancer detection and reduction in recalls during three consecutive annual DBT screening rounds, but the observed decline in interval cancers was not statistically significant.
"A study with longer follow-up and more screening rounds would be required to estimate the degree of overdiagnosis," Skaane and colleagues noted. "It is important, however, to keep in mind that 'overdiagnosis' does not diminish the benefit of mammography in decreasing breast cancer mortality."
Tomosynthesis increases cancer detection while reducing false-positive recalls, and because the greatest harm of overdiagnosis is overtreatment, the goal should not be fewer cancer diagnoses, but better treatment decision tools, according to the authors. Furthermore, additional studies with more rounds may be required to determine the long-term benefits of DBT screening, they concluded.