Optimizing radiation dose in whole-body CT polytrauma cases represents an ongoing battle, but it can be won, according to researchers from Oxford, U.K. To minimize risk to patients, the justification criteria must be robust and documented justification should be clearly communicated between the trauma team leader, CT radiographer, and radiologist, they emphasized.
In an audit of all 56 whole-body CT investigations performed in November 2016, nearly half of the scans were negative for trauma, and this is a serious concern, given the relatively high dose, explained Dr. Ahmed Elzein Mohamed and colleagues from the department of radiology at Oxford University Hospitals National Health Service (NHS) Trust.
Their audit showed that the reporting accuracy is very high at Oxford, with no major discrepancies and 84% agreement with the preliminary report by a registrar (i.e., a qualified medical doctor receiving advanced training in radiology). The average time from scan to report was within the one-hour target set by the Royal College of Radiologists (RCR), but the authors acknowledge the use of the mean as a timeline benchmark is "disingenuous." In future audits, they plan to measure the proportion of scans reported after one hour.
The average dose of 30.7 mSv was within normal limits, representing an increased relative risk of inducing a fatal cancer of 0.3% in a 20-year-old woman, the group said. Electronic requesting is preferable, but they displayed an RCR-approved example of a paper request form, which is shown below.
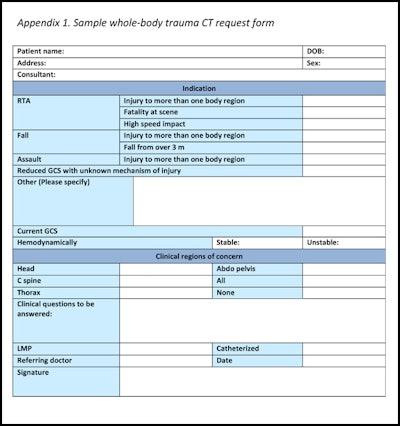

Example of a clinical justification form approved by the Royal College of Radiologists. DOB = date of birth, RTA = road traffic accident, GCS = Glasgow Coma Scale. LMP = last menstrual period.
All data were obtained from the hospital's RIS and PACS. Data were collected on adequate clinical information to justify the scan, request authorized by a radiologist or requested by a trauma team leader, artifacts, arm position, radiation dose, time to report, report accuracy, negative scans for trauma, documented primary survey, and use of additional abdominal or chest radiographs before CT; the RCR states if there is an early decision to request a trauma CT scan, then focused assessment with sonography for trauma (FAST) scans or plain films should not cause any delay.
The group's key findings were the following:
- Adequate clinical information to justify scan was present in 82% (46/56) of cases.
- Additional chest radiographs were performed before CT in 63% (35/56) of cases.
- Additional pelvic radiographs were performed in 54% (30/56) of cases.
- Arm position was down in 91% (51/56) of scans, and 70% (36/51) had streak artifact across the abdomen (p ≤ 0.02).
- The average time to report was 59 min, range 10 min to 175 min (standard deviation ± 35).
- There were no major discrepancies. The minor discrepancy rate was 16% (9/56). The consultant/senior radiologist agreed with the preliminary report in 84% (47/56) of cases.
- Around 45% (25/56) of scans did not have any significant sequelae of trauma.
- Mohamed and colleagues noted they compared the results with the RCR's 2015 guidelines, Standards of Practice and Guidance for Trauma 1 Radiology in Severely Injured patients. The primary survey was not documented electronically in any cases.
Take home messages
Whole body CT is requested frequently in major trauma centers, but these investigations are very resource-intensive and time-consuming. They subject the patient to a significant dose of ionizing radiation, so they require careful attention. But whole-body CT should only very rarely be delayed for chest or pelvic radiographs because radiographs are unlikely to alter clinical management, they said.
"Artifacts from medical equipment or arm position can be a limitation to whole-body CT reporting accuracy," the researchers continued. "Upper abdominal streak artifacts can be reduced by raising one or both arms or moving the arms away from the skin."
Also, a written primary survey report should be issued immediately, with an electronic record uploaded to RIS or PACS, so that it is available to both the clinical team and other reporting radiologists. A final report should be provided in less than one hour in all cases. It is acknowledged that reporting time does not follow a normal distribution.
The team's other tips include the following:
- The trauma team leader should be clearly identified on the justification form (electronic/paper).
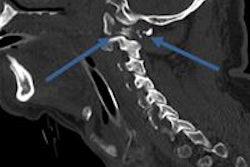
- Investigate whether it is possible to further optimize CT dose using improved neck stabilization equipment.
- As much clinical information as possible is required for justification. This is likely to facilitate quicker and more accurate reporting, and clear justification criteria assist direct communication with the radiographer.
Overall, for whole-body CT to be effective, there are several key aspects of the process that should be optimized, including appropriate justification, adequate clinical information, minimizing delay, minimizing dose, and image optimization.
As a result of this audit, the provisional primary survey report will be introduced at Oxford University Hospitals NHS Trust, they concluded.
The group's full presentation at the 2017 meeting of the European Society of Musculoskeletal Radiology (ESSR) in Bari, Italy, is available in the European Society of Radiology's EPOS database. To view it, click here.