European experts in molecular imaging expect the addition of cadmium zinc telluride (CZT) digital detector technology, advanced quantification software programs, and novel radiotracers in SPECT and PET imaging will lead to major advances in research and clinical applications for cardiovascular disease.
Cardiovascular disease is a serious health issue across Europe, with estimates of more than 49 million people afflicted with the condition, and that represents a 32% increase for men and a 26% increase for women over the last 25 years. Such rapid growth underlines the need for radiologists and cardiologists to diagnose and treat patients in an accurate and timely manner, and the diagnostic options include PET and SPECT imaging, with the addition of quantification methods.
To discuss the evolution and advance of cardiac PET and SPECT, GE Healthcare recently hosted a webinar to obtain the insights of two specialists on the modalities' growing contribution in cardiology with advances in technology, access to radiotracers, and changes in reimbursement procedures.
John Prior, PhD, CHUV University Hospital
 John Prior, PhD, CHUV University Hospital.
John Prior, PhD, CHUV University Hospital.John Prior, PhD, professor and head of nuclear medicine and molecular imaging at CHUV University Hospital in Lausanne, Switzerland, is considered one of the pioneers of cardiac PET/CT in Europe. His facility operates a rubidium generator that provides the radiotracer for more than 350 contrast-enhanced cardiac PET/CT studies per year.
Rubidium-PET/CT offers a relatively short scanning protocol of approximately 25 to 30 minutes to acquire dynamic left ventricular ejection fraction and cardiac-related results. Both cardiac PET/CT and SPECT exams can be performed on an outpatient basis with a relatively low radiation burden of approximately 1.8 mSv, he explained.
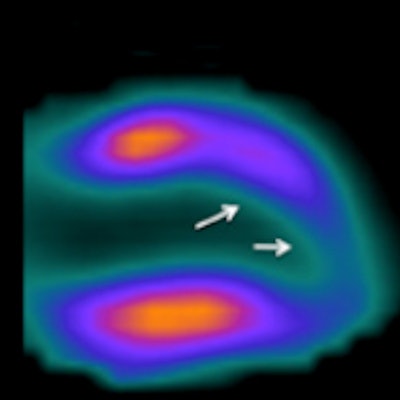
The scans can be performed with increasingly advanced quantification software programs designed to lessen the need for user interaction and to provide good reproducibility with excellent agreement for both global and regional myocardial blood flow and myocardial blood flow reserve. One key myocardial blood flow measurement targets the epicardial vessels, which often are the location for a stenosis.
"You also get a more accurate assessment of ischemia burden in patients with intermittent coronary artery disease," Prior said. "This is a very important step into treating high-risk disease patients and the lower-risk patients. It also helps in the clinical management of these patients."
For example, an ischemic burden of more than 10% in the whole myocardium is likely to prompt clinicians to recommend an invasive coronary angiography procedure. Also, decreased micro blood-flow reserve is likely to result in a cardio angiogram for these patients, he added.
"If there is quite normal myocardium blood flow reserve, then you would have a good prognosis without any need for another examination for the next three years," Prior said.
Quantitation adoption
In order for cardiac PET/CT with quantification to reach its full potential, more studies that prove its value in outcomes-based on decision-making are needed, he predicted.
"Is the patient in a better shape? What is the outcome with therapy-guided treatment? These would be relatively important questions to solve," Prior said. "We need multicenter trials to do that. We also need to use more widespread physician and technology education on what cardiac PET is, especially with full quantification."
And what about the influence of PET/MRI? Prior sees the hybrid modality as an "enhancement to the research side of clinical cardiology. The research still needs to be performed, but I don't think it is ready yet to enter the clinical arena. Something that is closer to enter the clinical arena -- and already has entered it -- is, for instance, quantification, but it also can be done with SPECT scintigraphy."
Dr. Frank Bengel, Hannover Medical School
Dr. Frank Bengel, director of the nuclear medicine department at Hannover Medical School in Hannover, Germany, emphasized the value of indirect effective methods to identify severe myocardial ischemia, such as left ventricle dilation or left ventricular function.
 Dr. Frank Bengel, Hannover Medical School.
Dr. Frank Bengel, Hannover Medical School."The perfect way to identify this would be to be able to look at absolute myocardial blood flow," he said. "This is something that has been established for PET already."
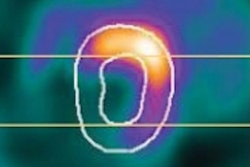
To do so, a clinician would have to acquire dynamic images within very short time frames after tracer injection. The process would be used to create time activity curves both for the tracer within the myocardium and the tracer within the arterial blood. The time activity curves could be fitted to compartmental models appropriate for the tracer to obtain a wash-in rate, which in turn translates into myocardial blood flow.
"The requirements for this are that first we need a tracer with high first pass extraction; then we also need scanners that have high temporal resolution," Bengel continued. "Of course, we need a well-defined relationship between the image signal and the tracer concentration, which is something that we have established for all of our myocardial perfusion tracers."
CZT detector technology
Today the best way to quantify myocardial blood flow is through SPECT imaging with CZT digital detector technology, he noted.
"The beauty of this is that CZT detector technology is very fast, because it is a very sensitive system, which takes images from the heart in multiple projections at the same time unlike regular myocardial perfusion SPECT cameras," Bengel said. "This initially has been done to do fast myocardial perfusion imaging and has been shown that you can obtain a standard cardiac myocardial perfusion study that you would normally need to acquire over 15 minutes with a regular perfusion SPECT system within two or three minutes."
Currently available SPECT myocardial perfusion tracers also help in establishing shorter image acquisition times to perform dynamic imaging and quantification in conjunction with the CZT technology.
With the global coronary flow reserve, clinicians can predict which patient is at highest risk and can identify the patient who would benefit most from revascularization than from targeted stenting of one vessel, Bengel said.
"If you take this together with the relative regional perfusion images and left ventricular function that we get from gated SPECT imaging, it really provides a complete picture of the ischemic burden in patients with coronary artery disease," he added. "We need more data on this approach, but we hope that the absolute flow will truly improve not just the diagnostic per-person and the prognostic value of SPECT imaging, but also the guidance of effective therapy in coronary artery disease."
Appropriate tracers
This question remains, however: Which are the most appropriate tracers for these applications? Bengel said there are "downsides and upsides" to all tracers, noting that thallium-201 has a relatively high radiation burden, which also is a concern for SPECT imaging. On the other hand, thallium provides very good ejection fraction and flow characteristics as a perfusion tracer.
"In the current discussion about radiation exposure, I think we should do fine with technetium-labeled tracers," he added. "Quantification of myocardial blood flow works with technetium-labeled perfusion tracers quite well. So I think those are tracers we should go with, because they result in less radiation exposure for the patient."
Combining cardiac PET with CT angiography also might help in the assessment of patients with cardiovascular issues, Prior suggested, especially given the capabilities of the newest PET/CT scanners.
"I think this would make sense, as the patient would be there and both examinations are available on the same machine," he said. "Depending on the risk of the patient, if it is low risk, you could do a CT angiography first. Then, if it is high risk, do a PET perfusion study."
Evidence-based research
Again, multicenter trials would need to be conducted to develop the evidence that choosing one pathway or another would result in a better outcome for the patient and be cost-effective, according to Prior.
"You also could pursue a stepwise approach," Bengel said. "You can probably have your cardiac CT as a first step at one institution. If it is abnormal, you can bring your cardiac CT to the PET or SPECT facility, which would have software tools available to perform a fusion of the CT with the nuclear studies to get more information on the localization of the disease and potential therapeutic targets."
Of course, to some degree, imaging choices are made in part relative to reimbursement. Both cardiac PET and SPECT are reimbursed in Switzerland, Prior noted, while in Germany there is no established mechanism to reimburse for rubidium- or ammonia-PET scans.
"We have high hopes that with novel fluorine-labeled PET perfusion tracers, the data will come in and ultimately lead to reimbursement," Bengel said. "SPECT is fully reimbursed, but there is no additional reimbursement for absolute quantification of blood flow."