I am training to become a cardiologist at the University Hospital Würzburg in Germany, and cardiovascular MR (CMR) has given me the opportunity to get a closer insight on heart diseases, including functional and morphological changes. During the past year, I have conducted approximately 800 examinations on a 3-tesla scanner, primarily on patients with suspected myocardial infarction or inflammation. I am absolutely fascinated by its capabilities.
For many colleagues, CMR is an almost magical device that is supposed to answer all our remaining clinical questions. Therefore, I was rather surprised to find out that, for example, stenotic heart valves are better explored by echocardiography. Today, with experience, it is much easier for me to choose the best cardiac imaging method for a patient, although after having acquired many new skills, I am still studying and trying to improve my knowledge day by day.
 Dr. Sven Piepenburg performs around 800 cardiac MR exams a year.
Dr. Sven Piepenburg performs around 800 cardiac MR exams a year.We have tried hard to optimize the MR images of our patients, but the difficulties of respiratory compliance and arrhythmia have limited our success. Detecting scar tissue is one of the most common tasks, and CMR not only reveals the existing damage but also can help to plan further interventions. Signs of inflammation or storage diseases are also often requested, next to a precise volumetry of valvular insufficiencies.
Traditionally, MRI has been in the hands of physicists and radiologists, yet cardiologists with MRI experience can help to set a different focus on a patient's heart disease, especially when all clinical modalities are taken into account. Cardiologists interpret imaging reports in the context of other diagnostic findings (echo, heart catheter reports, etc.) and use CMR to answer specific remaining questions, leading to better therapy.
Our scanner is an Achieva 3-tesla (Philips Healthcare) machine. It was upgraded from a 1.5-tesla system in October 2015. A higher resolution of images and shortened examination times were important factors for this update. We only use it for cardiac imaging done by cardiologists (the MRI is part of our cardiology department of Medical Clinic I). Originally, it was meant to be a research scanner, but it has become more and more an instrument of daily clinical practice due to the growing demand of our own clinic and outpatient facilities and practices.
Patient selection and techniques
Due to limited resources, good clinical practice is necessary to identify patients who actually profit from a CMR scan. Patients are suitable if they fit our scanner (60 cm in diameter, including a body coil on top) and they can follow our breathing signals and lay flat on their backs for 45 to 60 minutes. We also check for allergies, kidney and liver dysfunction, tinnitus, claustrophobia, tattoos, metal implants, devices, and signs of former operations. If necessary, more medical records are collected to rule out possible complications with MRI.
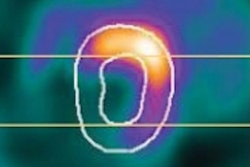
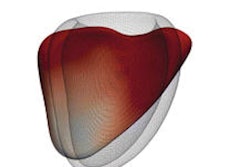
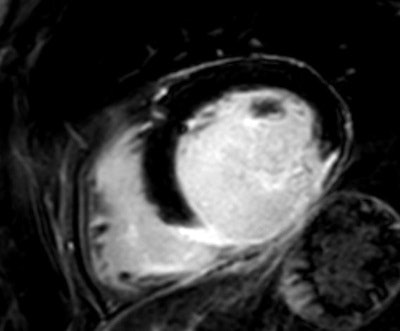 A 59- year-old man with acute myocardial infarction: late enhancement inferior and inferolateral, basal to apical, accompanied by a slight contrast substance enrichment of the pericardium.
A 59- year-old man with acute myocardial infarction: late enhancement inferior and inferolateral, basal to apical, accompanied by a slight contrast substance enrichment of the pericardium.In my practice I have certainly gained more knowledge in working with CMR, and I continue to get more ideas about how to use it to answer specific questions, such as late enhancement for detecting scar tissue, T2-weighted imaging for edema, short axis view, and aortic and pulmonary flow for precise volumetry.
The cardiologist's view is not only helpful to detect patients in need, but also to consider future therapeutic consequences and interventions. Therefore it seems to be essential for cardiologists to get training in advanced imaging like CMR. There is a rapid development of new techniques with better resolution and shortened examination times that allow us to perform more and more scans; however, we must not forget that our results should be of clinical significance too.
Our contrast agent is Gadovist, which we use for all late-enhancement images, and so far we have had almost no allergic reactions. Use of a contrast agent is essential for almost all our patients undergoing CMR, except for very few cases involving particular interests in functional and volume changes of the heart.
Looking to the future
Overall, the challenges and expectations are high, and I have certainly gained a more profound understanding of cardiac physiology and also of the technical limitations of our scanner. CMR adds further information to our patients' heart functions that is otherwise often impossible to receive in another way.
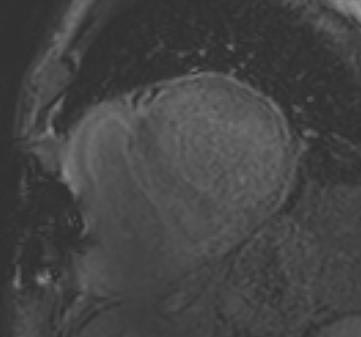 A 78-year-old man with cardiac amyloidosis: Nulling of "normal" myocardium is impossible, typical for storage disease. A PET/CT scan confirmed the diagnosis.
A 78-year-old man with cardiac amyloidosis: Nulling of "normal" myocardium is impossible, typical for storage disease. A PET/CT scan confirmed the diagnosis.The demand for CMR exams increased a lot during my first year of using CMR, and our team is already in need of reinforcement. In the future, we will probably have to handle more and more patients and we are therefore expanding our staff and starting to train more colleagues.
CMR will certainly play an even bigger role in the future and help to improve the individual health of our patients. We are also collaborating with other disciplines like nuclear medicine and radiology, and I am really looking forward to intensifying our relations to optimize clinical imaging for all our patients.
Dr. Sven Piepenburg is based at the Comprehensive Heart Failure Center and Department of Medicine I at University Hospital Würzburg in Würzburg, Germany.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.