Breast indications for MRI differ vastly across Europe, but techniques are closer to U.S. practice than anticipated, according to a new survey presented for the first time at the European Society of Breast Imaging (EUSOBI) annual meeting, which ended in Paris on Saturday.
The survey, which forms the basis of a paper to be published after Europe's biggest breast imaging meeting, reveals that big discrepancies exist between northern and southern European countries in who is selected for breast MRI and how MR is used, according to lead author Dr. Pascal Baltzer, consultant breast radiologist at Vienna University Hospital.
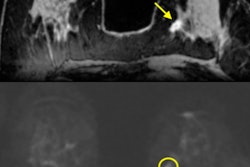
 Case 1: On a 44-year-old woman, MRI was performed for problem-solving due to suspicious lesion left side retroareolar region, several similar lesions on ultrasound, appearing hypoechogenic with dorsal acoustic shadowing. MRI shows dehydrated proteinaceous fluid on precontrast T1-weighted imaging, after contrast media injection a periductal enhancement. This is typical periductal mastitis and cancer could be excluded. All images courtesy of Dr. Pascal Baltzer.
Case 1: On a 44-year-old woman, MRI was performed for problem-solving due to suspicious lesion left side retroareolar region, several similar lesions on ultrasound, appearing hypoechogenic with dorsal acoustic shadowing. MRI shows dehydrated proteinaceous fluid on precontrast T1-weighted imaging, after contrast media injection a periductal enhancement. This is typical periductal mastitis and cancer could be excluded. All images courtesy of Dr. Pascal Baltzer.Speaking to AuntMinnieEurope.com, he confirmed the survey had thrown up surprising results. Given his experience of working in Germany and Austria, and close collaborations with Italian colleagues, Baltzer noticed there were significant differences, both in application and reimbursement of MRI. This prompted him to send an online survey to EUSOBI members between 1 November and 31 December 2015.
Survey questions covered which indications were paid for and which diagnostic and interventional techniques were used. It generated responses from 189 individuals -- of these, 163 were certified radiologists and 26 were residents, fellows, or doctoral candidates. Completed surveys came from 23 countries and partially completed surveys came from 34 different countries.
"Although the role of breast MR as a preoperative staging or problem-solving tool is hotly disputed, to our amazement we discovered that all respondents used it as both -- and that in academic centers it also served as an additional screening tool for high-risk individuals," Baltzer said. "In terms of differences, southern European countries, typically with lower healthcare budgets, use breast MRI more broadly than northern countries, which have stricter indications. In northern Europe, MR is predominantly used for young, dense breasts and invasive lobular cancer staging, whereas in Italy, Spain, Portugal -- and also Austria -- doctors tend to do what they think will work: This might include staging invasive ductal cancer or imaging a 50-year old with fatty breasts."
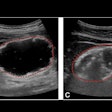
 Case 2: A 47-year-old woman with new palpable finding in the left lateral breast with architectural distortion in ultrasound, no suspicious microcalcifications. Problem-solving MRI showed no enhancement in the indicated region, thereby excluding malignancy. STIR = short tau inversion recovery.
Case 2: A 47-year-old woman with new palpable finding in the left lateral breast with architectural distortion in ultrasound, no suspicious microcalcifications. Problem-solving MRI showed no enhancement in the indicated region, thereby excluding malignancy. STIR = short tau inversion recovery.He added that breast MRI required more stringent justification when it came to reimbursement issues. In Germany, insurance is paid on a case-by-case basis after written request, whereas in Austria, MR is fully integrated in the screening program and is fully reimbursed in clinical routine when used as an extra imaging technique.
"In Austria and Italy, if a mammogram reveals asymmetric density then the next routine step is an MR because if it is negative there is no need to do a biopsy," he noted. "Northern country health systems such as the U.K. and Germany are more evidence-based, even if this is preliminary evidence. In southern countries and Austria, preliminary evidence doesn't preclude use."
Generational factors
Baltzer and colleagues also found a generational difference in the use of multiparametric MRI, particularly the application of diffusion-weighted imaging. Younger breast radiologists showed themselves to be more comfortable with quantitative techniques than the older radiologists who favored standard contrast-enhanced MR.
The group unexpectedly found no differences between Europe and the U.S. in terms of technique tendencies. The majority of respondents used fat-saturated T1- and T2-weighted imaging and agreed unanimously that the most important MRI technique was contrast-enhanced imaging.
"I hope that northern Europe will follow the latest paper on MRI problem-solving published in PLOS One in August that showed that MRI's diagnostic performance for cancer exclusion in noncalcified lesions is as good as biopsy. The study also showed specificity of 89%, and PPV values of 56%. These results may help change problem-solving practice," Baltzer said. "MRI can exclude malignancy and its sensitivity for additional findings does not mean it is a 'problem maker.' "
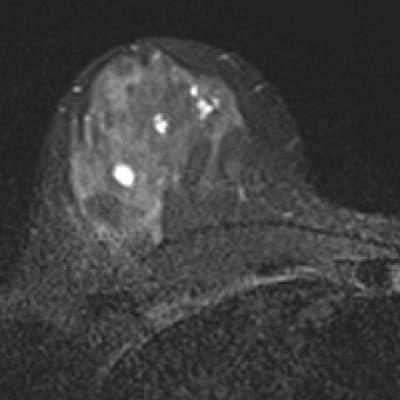
 Case 3: A 51-year-old woman with discharge on the left side and a suspected papilloma on the left side. Problem-solving MRI revealed a carcinoma on the right side BI-RADS 5 that was missed both by mammography and ultrasound.
Case 3: A 51-year-old woman with discharge on the left side and a suspected papilloma on the left side. Problem-solving MRI revealed a carcinoma on the right side BI-RADS 5 that was missed both by mammography and ultrasound.The issues surrounding equipment needed for wider routine use of breast MRI will also differ across Europe, according to Baltzer. In Austria, as in Hungary, Slovakia, and Italy, a proportionally higher number of scanners or examinations per population compared with other member states, translates into MR exams that are half the cost of those performed elsewhere, such as in Germany.
He believes it is important for specialists to discuss the discrepancy of MRI justification versus nonjustification across member states, as well as the generational issue of technique.
"The survey may instigate a debate about whether DWI [diffusion-weighted imaging] should be included in EUSOBI's guidelines on breast imaging and EUSOMA's (European Society of Breast Cancer Specialists') view on problem-solving. There is a lot of evidence on the usefulness of DWI and such quantitative criteria goes hand in hand with quality assurance," Baltzer noted, pointing out that he hoped to see wider use of DWI as an integral part of breast MRI because it is fast, simple, and robust. "In addition, the fact that there is no difference between a 'European technique' or a 'U.S. technique' bodes well for collaboration between breast imaging societies on each side of the Atlantic."
Combined mammography and ultrasound
On a different tack, Dr. Thomas Helbich, vice chair of the department of radiology and nuclear medicine at the Medical University of Vienna, covered the issues of combined mammography and ultrasound screening in Saturday's session, the "Best way to screen" debate.
The increase in sensitivity undoubtedly improves early breast cancer detection, however, the drawbacks are more recalls and more unnecessary biopsies, he stated. With respect to benefit, harms, and costs this means that ultrasound averts 0.36 (less than a half) of breast cancer deaths and gains 1.7 quality-adjusted life years (QALYs), he explained, citing a 2015 U.S. study by Sprague et al (Ann Intern Med. 2015, Vol. 162, pp. 157-166).
He also pointed to 354 more biopsy recommendations after a false-positive ultrasound result per 1,000 women with dense breasts compared with biennial screening by mammography alone. Furthermore, supplemental ultrasound for only women with dense breasts costs $246,000 U.S. (219,000 euros) per QALY gained.
"Ultrasound increases cost substantially while benefits are small," Helbich told AuntMinnie Europe.com. "Since 2014, Austria has been running such a screening program. We are in the process of recruitment and no data are available. However, based on one state (Tyrol) we can expect similar benefits/harms as seen in the study by Sprague et al."
He believes that while density of the breast should be considered, supplementing mammography with ultrasound is only one among several other options.
"In the future, breast cancer screening will go in the direction of personalized medicine pending on risk factor stratification," he said. A possible scenario in an optimistic projection for 2025 when considering imaging would be as follows:
- High-risk patients (life-time risk > 20%): MRI only
- Low risk, density 1: 2D-mammography only
- Intermediate risk, density 2 and 3: 3D-mammography (tomosynthesis), alternatively 2D-mammography combined with ultrasound
- High risk, density 4: MRI only
Alternatively, another scenario for 2025 with very conservative consideration of benefits, harm, and costs is mammography screening, if at all, he said.
"In this context, we should not forget the very promising role of cancer screening with liquid biopsy," he said. "This would mean no imaging but cancer markers via blood."