Achieving a fully integrated national RIS/PACS network using a single archive is a hugely challenging task, but it can be achieved with adequate resources and close cooperation between medical disciplines, according to researchers from the Republic of Ireland.
The implementation of the national RIS/PACS implementation scheme for Ireland represents a significant milestone in the development of a national electronic health record, providing a nationwide image archive for the health system, noted the authors of two e-posters presented at last month's RSNA 2014 meeting.
"The project has set new standards in aspects related to large system procurement and implementation," stated lead author Yvonne Goff, project manager at the National Integrated Medical Imaging System (NIMIS). "Confidence in the project has continued to increase as sites go live. Users are happy with the solution, particularly the PACS element, and despite early resistance, sites have been very engaged."
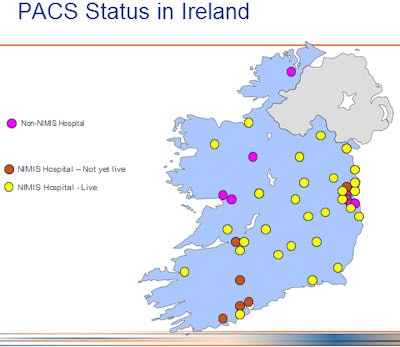 PACS status in the Republic of Ireland. Image courtesy of Yvonne Goff.
PACS status in the Republic of Ireland. Image courtesy of Yvonne Goff.The project's rapid implementation process has put pressure on the sites, as well as its vendor and the NIMIS team, and the five-year scheme has highlighted other gaps in the healthcare IT infrastructure, such as the current lack of implemented national order comms (OCM), results acknowledgement, and critical findings solutions, she admitted. However, a range of product developments have been identified by hospital staff, particularly on the RIS side, and vendor support has been excellent.
Ambitious project
In 2007, the Health Service Executive (HSE) in Ireland initiated NIMIS, the initial aim being to install a RIS/PACS solution into all publicly funded hospitals in Ireland. The first site went live in June 2011, and as of November 2014, 35 sites were live, or more if you consider satellite sites, explained Goff, Keith Morrissey, radiographer lead of the NIMIS project, colleagues. There are a total of 23,000-plus users, about 6,000 of whom are active, and there are more than 7 million studies in the archive, with more than 7,500 per day still being added. There are 10 million reports and more than 4 million orders on the system, making it the largest RIS/PACS in the world, they claimed.
| Current status NIMIS nonradiology imaging areas | |
| NIMIS live | 34 sites |
| Cardiology (differing activity component -- echo, ultrasound, cath lab, resting ECG, other cardiac investigations) | 14 sites |
| Obstetrical ultrasound | 8 sites |
| Vascular imaging | 4 sites |
| DEXA (nonradiology managed) | 3 sites |
| Pulmonary function | 2 sites |
| Dental imaging | 2 sites |
| Arthroscopy | 1 site |
| Radiotherapy CT planning | 1 site |
Before implementation of the NIMIS, there were 52 hospitals in the health service, of which only 15 had PACS. Except for some teleradiology systems for image transmission to the neurosurgical and spinal national centers, none of the existing PACS could communicate with each other. Today, NIMIS is handling 6 million images and reports, with 35,000 studies added each week to its central archive. A total of 31 sites are currently live on the system and one site a month is being added.
The main objective was to become "filmless" and "paperlite" in radiology, explained the authors. They hoped this would lead to a reduction in report turnaround times, enable remote reporting, improve access and availability of patient information, reduce repeat examinations, improve cost savings related to x-ray film usage and management, and improve patient data security. Other hoped-for benefits included facilitation of clinical audits, enabling images to follow the patient through the care pathway, improved liaison with primary care, and better integration with radiation oncology centers. McKesson was selected as the preferred vendor.
The researchers pointed out that the lessons learned from the procurement process were:
Detailed technical and functional specifications are necessary, but of limited value. There were no fewer than 1,900 criteria.
The various scenarios proved highly differentiating of the vendors' capabilities.
User involvement in the review and selection of solutions is very beneficial for buy-in and acceptability of the project.
The "demo week" was hard for both the vendors and the team. Some vendors used it as a sales event for other procurements.
Defining timelines at the outset and sticking to them helps user support and vendor engagement.
The unforeseen benefits of NIMIS included pooled resources for upgrade testing prior to deployment; centralized management reporting processes; collective support and system maintenance issues/developments, etc.; pooled knowledge of system personnel (between sites and national team); collective bargaining for the funding of additional modules, as it is a shared single system; and single connection point into other national projects such as endoscopy.
Under the centralized system design, hospitals now communicate and cooperate in a new way in radiology. Standardized processes, such as not printing radiology reports, have been implemented, including electronic communication of radiology reports to general physicians.
The NIMIS team has also encountered firewall configuration issues and various IT network problems, and the lack of national patient identifiers has hindered aspects such as full cross-site ordering, reporting, and most importantly, multidisciplinary team meetings. Also, access to legacy PACS was a problem at the outset, making data migration difficult, but this has been overcome with the cooperation of legacy PACS vendors.
Going "paperless" is extremely difficult, the authors stated. The electronic ordering of radiology procedures has been implemented, but without full OCM functionality, issues can arise. No results can be achieved without proper acknowledgement, and change management does not always yield the required end results, as has been the case with CT vetting. Keeping the focus on areas outside of radiology can be problematic without a key driver in these areas.
Data protection, including visibility of patient data on a national basis, is a key aspect of the project, particularly the number of users seeing the data, although a greater concern for the authors was the number of users not seeing the data. To extend beyond the NIMIS, the non-NIMIS legacy PACS could be cross-enterprise document sharing (XDS)-enabled in order to exchange data with other hospitals. NIMIS could choose to XDS-enable other 'ologies to take advantage of the archive, and the repository could be used for storing other, nonradiology image data, they pointed out.
In another lesson, it's crucial that resource commitment from areas outside radiology that use imaging is secured before project commencement, and this is now set as an initial project milestone. Particularly important is obtaining the necessary clerical and administrative resources for these areas quickly, and a knowledge of referral and scheduling workflows is essential, as is close cooperation between the radiology NIMIS team and their colleagues from the nonradiology areas from project commencement.
Standard radiology workflows do not equal workflows in other image-producing areas, and it's very important that the current workflows in these areas are documented in the appropriate detail at the commencement of implementation. A significant learning curve existed for the NIMIS national team, and McKesson staff members with regard to gaining an understanding of workflows in these areas. Ensuring the acceptance of colleagues and avoiding the perception of external imposition are necessary steps.
Some imaging devices do not have DICOM capability, and thus require installation of a virtual DICOM printer software application to facilitate conversion of the data to DICOM format. This process is relatively cumbersome, and requires additional user steps, so it is wise to continue to explore the options of streamlining this workflow. Direct DICOM/HL7 transfer is the preferred standard. With DICOM capture of text-rich files like exam reports, there is a resultant display issue on PACS due to the predominance of text. At low screen resolution, significant image zoom is required to read text clearly.
Existing third-party, dedicated standalone reporting solutions deliver very rich custom functionality in many areas, but it was quickly discovered that NIMIS PACS was unable to replicate this level of dedicated functionality. These existing reporting systems (echo ultrasound, obstetric ultrasound, vascular imaging) continue to fulfill their primary reporting role in these departments. Exam reports produced are converted to DICOM and stored to PACS via DICOM virtual printer software.
In terms of system management, local department responsibility for "housekeeping" of their section of the system is stressed during implementation and during refresher sessions as the system goes live. It's important that local nonradiology lead personnel develop a continuing close working relationship with the radiology NIMIS team during implementation and for the post go-live period, but the authors try to avoid the scenario where local department NIMIS leads are overly dependent on the radiology NIMIS team.
Nonradiology NIMIS leads are given skill sets to undertake routine daily quality assurance tasks and perform routine troubleshooting of local issues. Also, nonradiology NIMIS leads are urged to develop a distinct relationship with the NIMIS support helpdesk.
NIMIS RIS is being utilized to provide enterprise OCM functionality due to the absence of a national OCM solution, and as a result, the requesting process is not as slick as that provided by dedicated OCM.
While NIMIS is inherently a radiology system, the original design and implementation has extended the boundaries of the solution into other imaging-type services such as cardiology, vascular, arthroscopy, obstetrics, and respiratory functions, according to the authors.
For cardiology, there is an indication that regional/national cardiovascular information system (CVIS) procurement is commencing and an understanding that such a system would replace NIMIS RIS on relevant sites, but NIMIS PACS would continue to archive for cardiac image data. An obstetric ultrasound national maternity system is commencing soon, and this will include electronic requesting and reporting of exams. It is envisaged that NIMIS PACS would play an image archiving role for this system.
A national ordercomms system will be rolled out in the next two to three years, and electronic requesting, results, and image viewing currently performed via NIMIS RIS will fall within the OCM system remit.
The legislative framework is now in place to support the introduction of a national patient identifier scheme. Implementation of an identifier scheme and use within NIMIS would deliver immeasurable benefits to all system users, including nonradiology imaging areas, and would deliver a true single national patient imaging record.
Another possible extension is to cooperate with colleagues in Northern Ireland, where there are multiple PACS networks installed by Sectra. The current NIMIS architecture is XDS enabled, allowing for cross-border sharing of data.