NEW YORK (Reuters Health) - Initiating mediastinal nodal staging of suspected lung cancer with endosonography, followed by surgical staging (mediastinoscopy) if needed, improves the detection of metastases and reduces the rate of unnecessary thoracotomies, compared with surgical staging alone.
These are the findings of a large randomized controlled trial released online today in the Journal of the American Medical Association.
In an e-mail to Reuters Health, first author Dr. Jouke T. Annema, of Leiden University Medical Center in the Netherlands, said, "For clinicians, the message is clear: nodal investigation of lymph nodes with endosonography is as least as good as the traditional surgical method (mediastinoscopy) but is less invasive and associated with significantly less complications."
The study involved 241 patients with resectable (suspected) non-small cell lung cancer (NSCLC) in whom mediastinal staging was indicated based on computed tomography or positron emission tomography scanning.
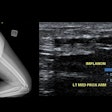
One hundred eighteen subjects were randomly allocated to surgical staging alone and 123 to endosonography (combined transesophageal and endobronchial ultrasound) followed by surgical staging in case no nodal metastases were found at endosonography. Surgical staging was needed in 65 patients in this group. Thoracotomy with lymph node dissection was performed when there was no evidence of mediastinal tumor spread.
According to the investigators, nodal metastases were found in 41 patients by surgical staging (35%), compared with 56 by endosonography (46%), and 62 by endosonography followed by surgery (50%).
This corresponded to sensitivities of 79%, 85% and 94%, respectively, the investigators say, with nearly identical negative predictive values -- 85% for endosonography alone and 86% for surgery.
"We expected that investigation of lymph nodes in the chest with endosonography would be (non-significantly) better in comparison to the traditional standard mediastinoscopy, as the endosonography techniques can reach more nodes in comparison to mediastinoscopy," Dr. Annema said.
In addition, "endosonography followed by mediastinoscopy (if negative) prevents unnecessary thoracotomy in one out of seven patients investigated," Dr. Annema reported. "The number of unnecessary thoracotomies will be reduced by half."
Given that the sensitivity of endosonography is similar to that of mediastinoscopy and that endosonography is associated with a lower complication rate, "endosonography should be the first step for mediastinal nodal staging," the authors conclude. "In clinics where endosonography is available, doctors already work like this," Dr. Annema told Reuters Health.
The fact that this study was conducted in tertiary referral centers is a limitation, the study team notes. Dr. Mark D. Iannettoni, the author of a linked commentary, agrees.
"Even though this emerging technology of endoscopic study can result in excellent results for predicting both positive and now improved negative results, highly skilled interventionalists are required to provide these exceptional outcomes," Dr. Iannettoni of University of Iowa Hospitals and Clinics, Iowa City, writes.
Dr. Annema said, "It is always a question of whether results obtained in expertise centers can be repeated in community hospitals. This also applies to the results obtained by mediastinoscopy."
But in Dr. Annema's experience, implementation of endosonography "goes very rapidly. Among others, we have shown that with a short dedicated implementation strategy, chest physicians who have never worked with ultrasound can obtain similar results as experts."
Still, Dr. Iannettoni cautions in his commentary that "until this modality can be reproduced at all centers where thoracic surgery is commonly performed, or until all of these patients are cared for at specialized centers, surgical staging must remain the gold standard for adequate preoperative evaluation."
By Megan Brooks
Source: http://link.reuters.com/nag86q
JAMA 2010;304:2245-2252.
Last Updated: 2010-11-23 17:35:27 -0400 (Reuters Health)
Related Reading
FDG-PET before RT can modify planned NSCLC treatment, August 11, 2010
PET/CT beats CT in NSCLC staging, but both have limitations, July 2, 2010
ASTRO: Use PET for NSCLC judiciously, November 3, 2009
Copyright © 2010 Reuters Limited. All rights reserved. Republication or redistribution of Reuters content, including by framing or similar means, is expressly prohibited without the prior written consent of Reuters. Reuters shall not be liable for any errors or delays in the content, or for any actions taken in reliance thereon. Reuters and the Reuters sphere logo are registered trademarks and trademarks of the Reuters group of companies around the world.